All it would have taken was to ensure that the children had a meal at night
Along with my colleagues, I had investigated the so-called mystery disease in Muzaffarpur, Bihar, during its outbreak in 2012, 2013 and 2014. The local name for it was acute encephalitis syndrome, but we found that the disease was not encephalitis but encephalopathy. This distinction is important. Encephalitis results from a viral infection, unless proved otherwise. The pathology is primarily in the brain. Encephalopathy is a biochemical disease, unless proved otherwise. The primary pathology is not in the brain. Specific treatment is scanty for viral encephalitis, but encephalopathy is eminently treatable.
Hypoglycaemia (when the level of glucose in the blood falls below normal) is usually due to an overdose of insulin in children with diabetes. It is easily corrected with oral sugar or intravenous glucose. The easily available 5% glucose solution suffices. Hypoglycaemic encephalopathy, however, is different from simple hypoglycaemia.
The disease pathway
We found that the disease broke out during the months when litchi was harvested, i.e. April, May and June. Muzaffarpur is full of litchi orchards. The illness started suddenly — children were found vomiting, displayed abnormal movements, were semi-conscious, and were convulsing between 4 a.m. and 7 a.m. The disease progressed fast — children went into coma and died within a few days. When sick children were tested, the blood glucose level was always below normal.
This disease was reminiscent of the Jamaican Vomiting Disease, a form of hypoglycaemic encephalopathy. It is triggered when unripe ackee fruits are eaten. These fruits contain a substance, methylene cyclopropyl alanine, which blocks a biochemical process called fatty acid oxidation, or gluconeogenesis.
There are two essential steps: gluconeogenesis is turned on and is then blocked midway by methylene cyclopropyl alanine. The back-up molecules of the unfinished process are certain amino acids that are highly toxic to the brain cells. Ackee and litchi belong to one plant family. My toxicology colleague, Dr. Mukul Das, found generous quantities of methylene cyclopropyl glycine in litchi fruit pulp.
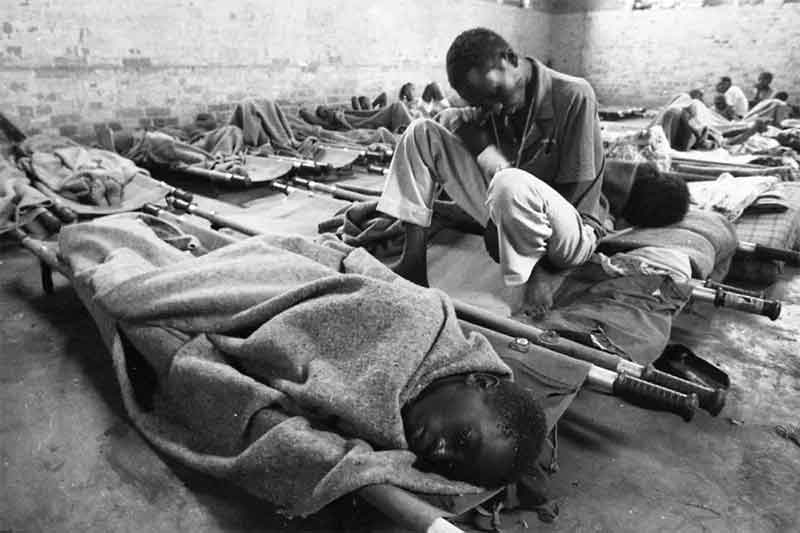
The disease affected only malnourished children between the ages of two and 10. A majority of them were from families camping in orchards for fruit harvesting. No child from the nearby towns fell ill. Children of well-to-do families never fell ill.
Litchi harvest usually begins by 4 a.m., which means that families are awake before that. They go to sleep early. If children go to sleep without dinner, parents usually do not wake them up and feed them. Litchis are collected in bunches and sent to the collection points, but single fruits fall to the ground. Children are free to collect and share the fruits with their friends.
With this information we made the hypothesis that the disease was hypoglycaemic encephalopathy. Along with my paediatric colleague, Dr. Arun Shah, we conclusively showed that the disease was indeed hypoglycaemic encephalopathy. With all the pieces in hand, we reconstructed the disease pathway.
After prolonged fasting, malnourished children slipped into hypoglycaemia in the morning. Since they had very little reserve glycogen in their livers, they were unable to mobilise glucose from liver glycogen, unlike well nourished children. The brain needs glucose as a source of energy. As a result of lack of liver glycogen, gluconeogenesis was turned on. Had there not been litchi methylene cyclopropyl glycine, the glucose levels would have been maintained, and the children would have come to no harm. As the children had consumed litchis the previous day, gluconeogenesis had been blocked, aminoacidaemia had developed, and brain functions had been affected. Hypoglycaemic encephalopathy had set in.
We were unable to demonstrate aminoacidaemia in children with hypoglycaemic encephalopathy, but that was done by investigators from the U.S. Centers for Disease Control and Prevention (CDC). The only missing piece in our studies was filled in by CDC colleagues.
Disease prevention
The disease can be prevented if children are well nourished, but that is not possible in the immediate term. It can also be prevented by ensuring that children eat a meal at night. All families were taught to provide a cooked meal to children before going to sleep at night. Preventing children from eating litchis is not easy, but the quantity of the fruit can be restricted with parental supervision. With all this health education, I was told that the disease number had come down drastically in 2016-18 compared to what it was in 2014-2015. I don’t know what went wrong this year.
In 2015, all primary health centres were supplied with glucometers to check the blood glucose levels of sick children. Doctors were instructed to take a blood sample for glucose estimation and, irrespective of the results, infuse 10% glucose intravenously. To correct mild hypoglycaemia, 5% glucose is enough, but here the problem is not hypoglycaemia alone, but aminoacidaemia as a result of blocked gluconeogenesis. To prevent any further back-up amino acid from accumulating, the fatty acid oxidation process has to be turned off quickly. That requires raising blood glucose level to abnormally high levels so that insulin secretion is stimulated, and that in turn turns off the gluconeogenesis.
What Dr. Shah and I found was that if ill children are infused with 10% glucose within four hours of onset of brain dysfunction, recovery is fast and complete. If only 5% glucose is given, or if 10% glucose is not administered within four hours, recovery is unlikely. I do not have detailed information from the field, but there seem to have been some human slip-ups this time.
Glucometers have not been maintained well. Health education was not sustained. New doctors are not familiar with all the information. Instead of 10% glucose, 5% is given. Children are taken mostly to private clinics and are then referred to the Sri Krishna Medical College in Muzaffarpur city since ambulance services are free of cost and easily available. Ambulances take more than four hours to reach the city hospitals from many rural clinics. We might think each error is minor, but when all the errors add up they contribute to deaths that should have been averted.
Dr T. Jacob John is a retired professor of virology from CMC Vellore
Originally published in The Hindu
Republished in public interest with the author’s consent