In 1896 a ‘plague’ pandemic arrived in the Indian city of Mumbai from Hongkong. Within a few days, strict quarantines have been imposed against Indian vessels at Suez and at many ports of Europe. Subsequently, strict quarantine measures were introduced in the city which included evacuation and burning of huts inhabited by the poor. There was an all-round clearance and alteration of indigenous dwelling units which were found insanitary by the British officials. Many buildings were destroyed or rebuilt. Slums were burnt and its poor residents were asked to be relocated by authorities. The city witnessed flight of over 10,000 people following the outbreak. Most of them who fled the city were poor working-class population. Financial allotments for sanitation work in all the Indian cities were dramatically increased after this plague outbreak. European officials started aggressively involving in sanitation improvements, as the plague outbreak badly damaged the East India Company’s trade interests across the globe.
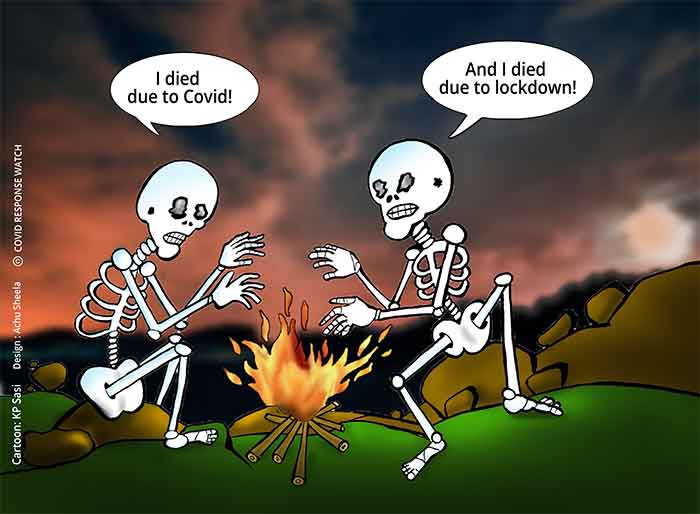
The response to pandemic outbreaks in the post-colonial India is also not very different from the colonial times as evident from India’s response in 1994 when there was an outbreak of bubonic and pneumonic plague in south-central and western India from 26 August to 18 October 1994. Containing the impact of the epidemic on commerce and the image of the country is still central to any discourse on epidemic control.
A new dimension added to the public health response by the corona pandemic is the need to deal with thousands of migrant workers in the cities. Immediately after the announcement of ‘lock down’ of the country due to Covid 19 pandemic, the mass exodus of migrant workers from the urban centres of India to the village hinterlands was widely popularised by the social media. Migration, in fact, is a natural characteristic of all ‘mammals’ as they migrate in search of greener pastures. The urban India woke up to this hidden reality with which they were living unaware for the past many decades. The sight of exodus of migrant workers has broken hearts of many of the urban elites. This has also brought deeper realities of distress migration, labour trafficking and bonded labour to the limelight.
I am also a migrant worker, living in Delhi for the past 30 years. I left the Kerala state of India about three decades ago in search of higher education and better job prospects. When I came to Delhi, there were several thousands of others belonging to my home state, staying in Delhi. Some of them continued to stay back in Delhi, but many of them further migrated to more developed Western and Gulf countries. The reality of my migration is very different from that of thousands of migrant workers who tried escaping the city in the aftermath of the current lockdown. Maintaining ‘social distance’ was not their felt need; rather escaping from an imminent death due to starvation in the absence of any remunerative work was their priority.
Magnitude of the Migrant Workers Problem
According to International Labour Organization, in 2017, over 41% of all international migrants were born in Asia and 17 million were from India – making India the largest “source country” for migrant workers. India is also the world’s largest source country for international migrant workers, with around 15.6 million Indian-born individuals living outside India. One out of every twenty international migrants originate from India. 50 million international migrants reside within the United States. Saudi Arabia, Germany, Russia, the United Kingdom and Northern Ireland together host 45 million international migrants.
Within India, people migrate from underdeveloped areas of states such as Bihar and Odisha to developed urban centres such as Delhi and Ahmedabad. Two out of every ten Indian citizens are considered an internal migrant. Many Indians also often migrate seasonally, based on labour demand and job availability. Most of these migrant workers are not employed like I do in the formal sector. Fortunately, I don’t belong to the group of migrant workers who were in the limelight due to the ongoing countrywide lock down in India. Sadly, many of my friends from the urban middle class became aware of their existence just now only.
Who are these Migrant Workers?
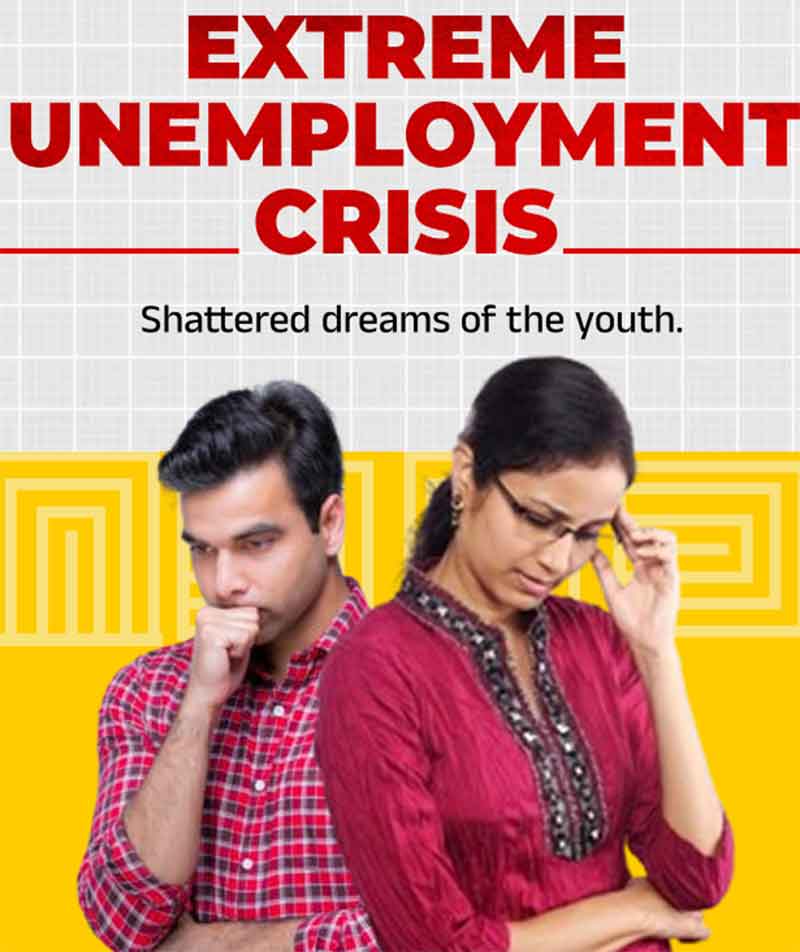
Migrant workers appeared in the highways during the early days of the lock down in India were unskilled labourers, employed mostly by the flourishing informal unorganized sector in our cities. They work as household servants, street vendors, sanitary workers, and support staff in industries. They receive daily wages, work without leave and social security and lead a ‘hand-to-mouth’ existence. Many of them work as ‘bonded labourers’ in the city and its extended surrounding agglomerations. Majority are unskilled, uneducated, and lack knowledge of local languages, laws and customs. Only a fraction of these migrants find employment in sectors consisting of higher-skills, and better-paying work. Most migrants accept offers of low paying seasonal labour, which lacks fixed working hours and is prone to wage fluctuation.
The demand for temporary migrant labour is widespread in India’s textile, construction, domestic work, brick kiln, transportation, mining and agricultural sectors, among others. Some scholars assert that as many as 100 million Indians are circular migrants (though India’s National Sample Survey estimate them as only 15 million). There is a lack of institutionalized regulation and an increased risk of exploitation of many of these labourers. Siddarth Kara, a well-known scholar on labour issues through extensive research in South Asia found that many of these labourers experience extreme poverty, belong to a minority ethnic group/caste, lack access to a formal credit market (due to a lack of any tangible assets or collateral for loans other than their labour), has little formal education and/or literacy, and often lack any other reasonable alternative to achieve economic stability.
Roots of Labour Migration
According to some sociologists belonging to the school of ‘Dependency Theory’, people are pulled out from underdeveloped ‘periphery’ regions to the developed ‘core’ regions – sometimes by choice and some other times by force. ‘Cores’ flourish as parasites by eating up resources including labour and raw materials from the peripheries. Such core-periphery transactions happen both internally and internationally.
Historically, migration in India was very low due to the prevalence of caste system, joint families, widely accepted traditional values, diversity of language and culture, lack of education and predominance of agriculture and semi-feudal land relations. Introduction of capital-intensive production processes in urban centres and breaking away from traditional social values and systems lured labourers from villages to cities. Lack of job availability in rural areas, extremely high or low levels of rainfall, lack of available land to cultivate, and local socio-political conflicts are some of the compelling factors for this internal migration in India.
Though millions seek to migrate for economic and other livelihood opportunities, many are coerced or deceived in the recruitment or transit process. As a result, many prospective migrant workers find themselves trapped by contracts or debts they are unable to pay back and in situations of labour trafficking and bonded labour. Caste is also influential on internal migration in India, as those from lower castes tend to be in more impoverished socioeconomic situations that necessitate internal labour migration. Estimates of people trapped in situations of labour trafficking vary from 20 million to 65 million people globally. Indian states are sources, destinations, and transits for men, women, and children vulnerable to labour trafficking.
Urbanization Aided by Availability of Cheap Labour
Economic hardships and environmental decline force the poor people to migrate to rich areas where they live through self-denial and poverty. Availability of cheap labour – both bonded as well as free variety is one of the leading causes of urbanisation, manifested by increase in population, presence of a booming construction industry, crowded dwelling units and overburdened public health services in the cities. These cities are unable to survive pandemics like Covid 19. Due to lack of financial and technical resources, many of the water supply and sanitation amenities are not properly maintained. All these lead to the high prevalence of water borne infections, especially diarrhoea in the urban centres of developing countries.
Life in dilapidated and congested structures in slums with fleas, bed bugs, ticks, flies and mosquitoes facilitate person-to-person transmission of conventional diseases TB, influenza etc. through micro-organisms of multiple forms and virulence. Majority of the urban health problems are actually “diseases of poverty” which include gastro-intestinal diseases, respiratory infections and chronic degenerative diseases – all associated with poor living and working conditions and disorders due to stress and social isolation.
In the cities and towns of developing countries, there is no proper sewerage system and untreated human excreta mix up with water in rivers and canals. Many people use backyard pit toilets and resort to open defecation, causing spread of hook worm, intestinal worms, typhoid, dysentery and diarrhoeal diseases. Accumulation of solid wastes due to lack of facilities for its disposal spread parasitic diseases such as leptospirosis due to garbage associated proliferation of insect and rodent vectors. Besides the age-old problem of faecal contamination, the water sources are contaminated by chemicals from industrial effluents, agricultural fields and even from domestic sewage.
Many studies on urbanisation wrongly concluded that urban life is conducive to good health as urban centres have more material and educational resources, physical security and access to medical care. Such a generalisation is not only contradictory to empirical evidence but also suffer from information gaps and biases. The statistical base of many studies, which attribute a better health status to urban dwellers is heavily weighted by the superior health status of the affluent city dwellers, as the poorest are statistically elusive due to their transitory or illegal migrant status and whose health statistics remain unrecorded. It has already been pointed out that the poor segments of urban communities are having a worse health status compared to the rural poor.
Public Health Scenario of Urban Centres
There is a critical ecological balance between humans, microbes, climate, land and water. Urbanisation disturbs this balance, if it proceeds by harming the optimal biological functioning of organisms in an ecosystem. A society cannot survive by exceeding the replenishment capacity of its ecosystem. The health experiences of man over the ages especially outbreak of plague, pestilence and famine are aided by disruptions in local ecologies. Recent outbreaks of mosquito borne diseases of Dengue and Malaria in the national capital region of Delhi was attributed to destruction of the ecology of this area due to rampant construction work triggered by the demand for dwelling units and office spaces precipitated by the liberalisation and globalization.
Consequence of urbanisation is manifested as poverty of a large segment of population who have little prospect for even marginally participating in the economic mainstream or improving their life chances. Its usual indicators are high infant mortality rate, low life expectancy, insufficient diet, limited access to health care, low levels of literacy and limited years of schooling. As the urban poor in the developing countries live at the interface between underdevelopment and industrialisation, their disease patterns reflect both the worlds and resemble a cocktail of communicable and non-communicable infections.
The ancient cities lived in balanced reciprocity with their surrounding countryside, by exchanging skills and money for food. But the urbanisation of the modern period was purely through exploitation of ecosystems for accumulating profit and expanding political and economic control. In 19th century Europe, urban centres were created by drawing people from rural areas where mechanisation of agriculture and aggregation of land holdings displaced and impoverished rural workers. They were lured into the cities with the promise of job but got crowded, filthy, insanitary dwelling spaces in return.
Lessons from Colonial Response to Public Health Challenges of Urban Centres
Europeans created coastal cities in the Third World, including in India to act as foci for trade. The crowded urban populations stimulated the evolution of those bacteria and viruses which are crowd dependent. It is to be noted that most of the epidemics which occur in urban centres are “hit and run events” because the microbe cannot withstand “the onslaught of the host’s anti-body response”. For example, measles attacks an individual only once, but can continue to circulate indefinitely by infecting the new generation children in a crowded urban centre.
Urban settlements facilitated rapid transmission of epidemics by constantly replenishing non-immune individuals either from the cohort of new-borns, or from the constant stream of visitors from other cities or outlying rural areas. According to McMichael, “the saga of human plagues is essentially the saga of decimations of urban populations – the plagues of Pharaonic Egypt, the Justinian plague of latter stage Rome, the Black death, Syphilis in 16th century Europe, tuberculosis, the post-World War I influenza pandemic.” etc It continued through the HIV (AIDS) pandemic which began in 1980s and today the Covid 19 pandemic. As large cities have sprawled mightily and huge urban conglomerations have formed, age old infectious diseases have proliferated among the crowded city dwellers.
Most countries of the Third World had a health service system in which the local traditional medicine and folk practices which took care of people’s health problems. When the colonialists systematically ruined the cultural roots of the colonies these traditional systems were also destroyed. The new health services system established by the colonisers was moulded essentially to maintain the colonial rule. Health services, established in urban centres served only the Europeans, army and the local elites who played a subservient role to the colonial masters. The minimal health services existed did not correspond to the health needs of the masses as the colonial health system was racially skewed and was focussed on curative services to benefit larger colonial interests.
The potential of the health services was further limited due to its irrelevance to the local culture. The preventive and sanitary measures were available only in the European quarters of the towns. As the nature of health services was mainly determined by the demands made by the rising political class (the urban educated middle class) and by the perceptions of medical bureaucrats, the services were never oriented towards the needs of the masses.
The response to public health emergencies of the colonial period in urban centres was mainly (i) the response of the administrators by creating local government in Indian towns and (ii) the response of the colonial preventive medicine. The establishment of local government in the town is prompted by (i) the concern about the insanitary condition existed in urban centres, (ii) the need to share the financial burden of the sanitary work with the local rate payers and the need to ensure the cooperation of the locals for the continuation of the colonial extraction. There was also a need to defend the state from accusations of exploitation.
Colonial preventive medicine responded by suggesting preventive inoculations, segregation of suspects, improvement over sanitary conditions, improvement in water supply and campaigns for mosquito eradication. It is to be noted that diseases like TB, which were chronic did not invite much attention (as they would not cause disruption in trade), while plague, smallpox, cholera, malaria etc. got all the attention of the colonial epidemiologists due to the probable adverse impact of these diseases in the trade front.
Thus, the responses of the colonial preventive medicine emanated partly from the discourse of economic efficiency of the colonial enterprise and partly due to its perception and concern about the huge sanitary problem posed by the natives. The measures taken against epidemics were to ensure uninterrupted export in the backdrop of various quarantine laws imposed on Indian ships followed by various sanitary conferences held in the last half of the 19th century.
Post-colonial Public Health Scenario in Urban Centres
Even after independence, the health services in most of the developing countries such as India continued to function in the same way it worked during the colonial period. Poor migrant workers are perceived as part of a bigger sanitary problem, as perpetrators of the pandemic and as illiterate, ignorant, troublemakers. The recent spraying of germicides on migrant workers who were cornered and lined up in the highways as part of governmental response to control the corona epidemic is an example of this perception by ruling regimes in Indian stats.
After independence, many super specialty hospitals have been established in the Indian cities. The entry of Transnational Pharmaceutical companies with various drugs and devices established the hegemony of the bio-medical paradigm of health care. They offered services and products for a price which a poor migrant worker can’t afford.
Migrant workers are perceived by businesses as entities without any purchasing power and these people remained out of their target marketing groups. These workers often did not have voting rights and hence they were ignored by political parties. They never had basic documents such as Aadhar cards and hence they remained out of welfare services offered by the governments. They maintained no bank accounts and therefore they were never benefitted by any ‘direct transfer to bank’. Thus, the health services in India and other similar developing countries are inadequate and ill equipped to meet the epidemiological challenges currently existing in these countries, particularly by migrant workers.
Re-imagining Public Health in the Post-Corona Societies
The process of urbanisation began from the stone age itself. When men ceased to be a ·hunter gatherer and started settlements and agriculture, diseases also began to occur in the form of epidemics. Conversion of forests into farmlands and construction sites created puddles where mosquitoes could breed. Domestication of animals in close proximity with the living space of humans resulted in sharing the pathogen pools and thus cattle gave TB and smallpox, horses gave common cold (through rhinovirus), Dogs gave measles (through rinder pest), pigs and ducks gave influenzas and now bats gave the Corona virus.
By 3000 B.C., there were large settlements in Babylon, Mesopotamia and in Indus Valley. These cities are raised through large scale agriculture in their hinterlands. Large scale settlements resulted in pandemics. According to Procopius, 40% of the population of ‘Constantinople city died in the Plague outbreak of A.D. 542. Trade, travel and war spread epidemics into new areas. Colonialism aggravated the epidemic outbreaks in colonies by precipitating famines through interference in the patterns of extraction and utilisation of indigenous resources.
As dependency theorists put it, urban centres in the developing regions of the world continue to be conduits of extraction from the hinterlands. The essence of urbanisation is nothing but over exploiting the resources of a hinterland and processing and utilising it by a minority, risking the wellbeing of a majority. The neo-colonial structures and institutions cannot escape from the charges of perpetuating ill health and underdevelopment.
Solutions for ‘urban decay’ and search for possibilities of ‘urban renewal’ must be based on strategies to minimise the parasitic growth of cities and to reduce the distress faced by rural populations. It is essential to attain ‘social’ and ‘economic development’ of both rural and urban areas – without compromising the need of resources of any section of the population who live either in the present or in the future. ‘Health transition’ in the post Corona era should be attained through broader social changes. Such a transition will be sustainable if effected through measures to improve economic and political control – not only of individuals and households but also of communities and nations.
As it is extremely difficult (if not impossible) to eradicate microbes as they would survive through “ceaseless evolutionary adaptations”, it would be better to equip the people with nutrition by eradicating ‘hunger’ via minimising the wasteful consumption of “urban elites” and maximising the essential consumption of the poor. It calls for redistributive measures through changes in fiscal policies at the national level and a revamping of institutional arrangements which sustain inequality.
Epidemiology should be freed from both business interests who are out there to make profit and from the ruling regimes who use it for social control. Towards that end, forces of democratisation are to be supported and encouraged. Social and political education of the masses, setting up of public distribution systems while simultaneously pursuing measures to improve the overall food and economic security of individuals, strengthening the health care infrastructure by integrating them with indigenous systems of medicine to take care of the needs of all sections of the population are suggested to attain the renewal of the public health systems in the post Corona world.
Finally, it is also time to revisit our good old Gandhi. In a letter to Jawaharlal Nehru (dated 5-10-’45) M K Gandhi wrote: “I am convinced that if India is to attain true freedom and through India the world also, then sooner or later the fact must be recognized that the people will have to live in villages, not in towns, in huts, not in palaces.“ In last century, M K Gandhi identified the problem with today’s urban migrant labourers. He believed: “Modern economic systems rooted as they are in self-indulgence, multiplicity of wants and divorce of ethics from economics are large-scale mechanized, centralized, complicated organizations. They are disfigured by unemployment, under-employment, pauperism, exploitation, a mad race for capturing markets and conquering lands for raw materials. They involve enslavement of the individual, treating man only as a hand feeding the machine, reducing him to a mere adjunct of the machine.” His solution was nothing but creation of self-reliant and safe communities in the country based on principles of truth and nonviolence. He wrote: “Village Swaraj is man-centred non-exploiting decentralized, simple village economy providing for full employment to each one of its citizens on the basis of voluntary co-operation and working for achieving self-sufficiency in its basic requirements of food, clothing and other necessities of life.”
I have no intention to suggest that we must go back to the same village system in India, which to a great extent was based on caste-based violence and feudal suppression. Indian villages have been considerably over romanticised by many authors as heavenly abodes of healthy people. In fact, many people started migrating to urban centres just to escape from the clutches of caste system, poverty and feudal oppression. We need re-imagining our villages beyond the caste system where individuals get opportunities to prosper and flourish. Let the inevitable crash of the economic order to be precipitated by the Corona virus in the coming days may help us to re-imagine our world based on equity and justice.
(Kandathil Sebastian is a social scientist based in Delhi. This article has borrowed many insights from his own PhD Thesis titled ‘Public Health and Urban Processes – A Study of Alleppey Town’ submitted to Jawaharlal Nehru University in 1998)
SIGN UP FOR COUNTERCURRENTS DAILY NEWS LETTER