Co-authored by K Rajasekharan Nayar, Anant Kumar, Arathi P Rao, and Lekha D. Bhat

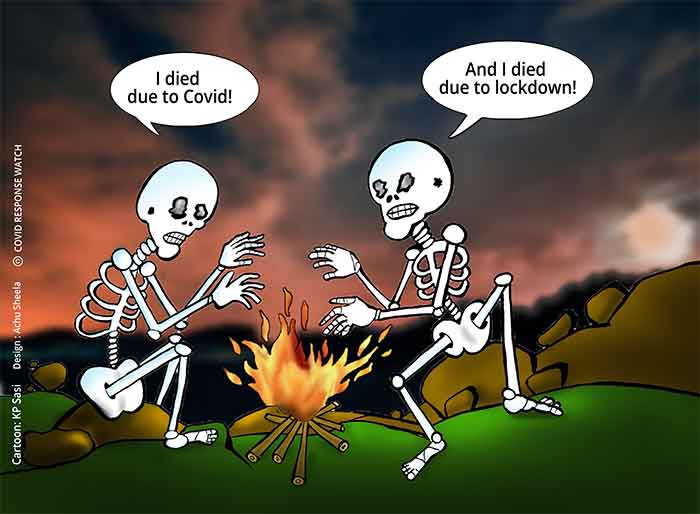
When unknown entities affect humans, they become unsteady especially during crucial times. This leads to ambiguous decision-making with respect to a number of key issues and factors. What happened when COVID-19 struck the world in the form of a pandemic is not different. A number of assumptions have played a role in prescribing preventive strategies for COVID-19.
It appears that the assumption of universality with respect to the behaviour of the virus is debatable. This universality is probably responsible for evolving and prescribing a homogenous model of prevention and control. A global perspective as suggested by some people is fine to some extent but it does not mean that the comparisons between nations and even some states in India with respect to success and failure of preventive strategies even by graphical presentations is desirable given the large unknown component regarding the virus. We still stand where we had been in 1918. And when that virus disappeared from the globe, scientists recreated it in the so-called safe environments of Centre for Disease Control Laboratories just to study the genome sequence and possibly develop vaccines. According to CDC, it was first identified in military personnel from the United States in 1918. At least 50 million people died worldwide with about 675,000 of the deaths occurring in the United States. For several decades, several uncertainties plagued the researchers and public health scholars. These included the questions about the origin of the virus despite it being erroneously called as Spanish flu, the questions about its deadly action and even about the differential impacts world-wide. Although recreated, many questions remain unanswered.
Subsequent pandemics were not related to the 1918 strain but many millions perished in the Flu pandemics which occurred in 1957, 1968 and 2009. Unlike the earlier pandemics and also the present COVID-19, the 2009 pandemic was slightly different. It largely affected the young population as they did not have any existing immunity (as detected by antibody response) to the (H1N1) pdm09 virus. A large number of people above the age of 60 had immunity against the virus ‘probably’ due to an exposure to H1N1 strain of the virus.
What we want to reiterate is the fact that the uncertainties continue to affect us in 2020 and therefore indecisiveness and ambiguities continue.
We are focusing only on the issue of preventive strategies which does not mean that ambiguity regarding other decisions may not exist. One of the key strategies recommended and enforced through legal measures strictly is the use of masks. And from the beginning, the ambiguity regarding the use of masks by the general public was evident with an opinion by many that such use by healthy people may not be necessary. The latest WHO advice brought out on June 5th 2020 reflects this ambiguity although this is now ‘masked’ with a pros and cons style.
WHO advises decision-makers to apply a risk-based approach focusing on some criteria when considering or encouraging the use of masks for the general public while the advisory is unequivocal regarding their use (both surgical or respirator masks) for health workers The risk assessment according to WHO should be based on several considerations such as risk of exposure such as intensity and epidemiological pattern of the infection especially community transmission and characteristics of the population and the setting in which population lives like density etc. It should be also based on the vulnerability of the population such as age and co-morbidities. The availability of different types of masks also needs to be considered but more importantly the feasibility of its use is also important especially when in many places adequate water is not available to clean the masks as use of unclean masks and repeated use of such masks will have more adverse effects.
The advisory also gives details about the ‘likely’ advantages and disadvantages due to the use with disadvantages superseding advantages. The essence of the advisory regarding this is that the possibility of self-contamination which may amplify the growth of microorganisms. Facial skin lesions, irritant dermatitis, acne, respiratory problems among the aged, headache etc. are some of the disadvantages reported by the WHO advisory. A false sense of security can also develop among users leading to lo adherence to other critical strategies like physical distancing, hand hygiene, etc.
The advantages on the other hand according to the latest advisory is the reduced potential exposure risk from ‘infected persons’ and also reduced exposure from people caring for the infected persons as well as a cultural expression of the need for preventive strategies. But the advisory suggests that without complying for other measures such as hand hygiene, not touching nose and mouth (this may also include spitting) and distancing, wearing masks may not be effective. The interim guidance is based on a WHO sponsored systematic review published in the Lancet which found no clear evidence of any intervention even when properly used, was associated with complete protection from infection unless complete adherence of other measures such as hand hygiene, physical distancing and even eye protection was followed (The Lancet, 2020). Overall, the WHO advisory is evidently ambiguous and conflicting without taking a clear position due to lack of clear evidence. It takes a safe position by suggesting the use of masks with conditions and a careful reading will reveal the fact that the advisory is unsure of giving a clear recommendation.
Earlier to this Lancet paper and the WHO interim guidance, many reports which appeared in May, 2020 except the Centers for Disease Control in the United States have been unsure of the advantage of face masks ((Davis, 2020; Carbone, 2020). The Centers for Disease Control and Prevention and some other reviews support the use of masks and face coverings and recommends the use of cloth face coverings to help and slow the spread of COVID-19 (CDC, 2020; Howard et al., 2020). The CDC suggest, “your cloth face covering may protect them, their cloth face covering may protect you” highlighting that wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies), especially in areas of significant community-based transmission may help in the containment of disease.
Overall, the scenario regarding preventive strategies is becoming hazier. The ambiguity continues to ride in COVID control and this has serious implications for decision-making. Although, WHO suggests decision based on risk assessment by respective governments and agencies, this may lead to an ad- hoc approach and the supremacy of non-technical know-all syndrome and of generalists. This only means that the political leadership has a major role who needs to act in conjunction with professionals who are familiar with the context in which the virus operates.
(K Rajasekharan Nayar is Professor at Global Institute of Public Health, and Santhigiri Research Foundation Thiruvananthapuram, Kerala, India. [email protected]; Dr. Anant Kumar is an Associate Professor at Xavier Institute of Social Service, Ranchi, India. [email protected]; Dr. Arathi P Rao is affiliated to Prasanna School of Public Health, Manipal, India. [email protected]; Dr. Lekha D. Bhat is Assistant Professor in the Department of Epidemiology and Public Health at Central University of Tamil Nadu, India. [email protected])
References:
Carbone, C. (2020). Report on face masks’ effectiveness for Coronavirus is dividing scientists. New York Post, May 7, 2020. Available at https://nypost.com/2020/05/07/report-on-face-masks-effectiveness-for-coronavirus-is-dividing-scientists/ (Accessed on June 4, 2020).
Centers for Disease Control and Prevention. (2020). Use of Cloth Face Coverings to Help Slow the Spread of COVID-19. Available at https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html (Accessed on June4, 2020).
Chu, D. K., Akl, E. A., Duda, S., Solo, K. et al. (2020). Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet, June 1, 2020. DOI:https://doi.org/10.1016/S0140-6736(20)31142-9. PMID32497510.
Davis, N. (2020). Reports on face masks’ effectiveness for COVID-19 divides scientists. The Guardian, May 4, 2020. Available at https://www.theguardian.com/world/2020/may/04/scientists-disagree-over-face-masks-effect-on-covid-19 (Accessed on June 4, 2020).
Howard, J. (2020). WHO stands by recommendation to not wear masks if you are not sick or not caring for someone who is sick. CNN, March 31, 2020. Available at https://edition.cnn.com/2020/03/30/world/coronavirus-who-masks-recommendation-trnd/index.html (Accessed on June 4, 2020).
World health Organization. (2020). Advice on the use of masks in the context of COVID-19: Interim guidance. WHO, 5 June 2020. WHO Reference Number: WHO/2019-nCov/IPC_Masks/2020.4. Copyright: CC BY-NC-SA 3.0 IGO. Available at https://www.who.int/docs/default-source/coronaviruse/corrigendum-to-ig-2020-4-ipc-masks-2020-06-05-pp-15-16-2020-06-06-e.pdf?sfvrsn=c5992b89_2 (Accessed on 7 June 2020)
SIGN UP FOR COUNTERCURRENTS DAILY NEWSLETTER