The U.S. Coronavirus (officially, Covid-19) cases have hit a record daily high as more than 83,000 new cases were reported in the U.S. on Friday.
At the same time, scientists have warned that the U.S. approach to fight the Coronavirus pandemic and the inconsistent use of masks to prevent virus spread could lead to the cumulative loss of more than half a million lives by the end of February.
US cases reach record high
The U.S. coronavirus cases have hit a record daily high as states grapple with a renewed wave of infections.
Citing data from local state health authorities, the U.S. Covid Tracking Project (CTP) reported 83,010 new cases on Friday.
The U.S. Surgeon General Jerome Adams has warned that hospital admission numbers are growing, but mortality rates are falling due to better patient care.
According to the CTP, nearly 8.5 million coronavirus cases have been reported in the U.S. since the pandemic began.
The daily increase on Friday surpassed by more than 6,000 cases the tracking project’s previous record of 76,842 on July 17.
Over the last week, the U.S. has tallied 441,541 new infections – its largest seven-day increase since the end of July.
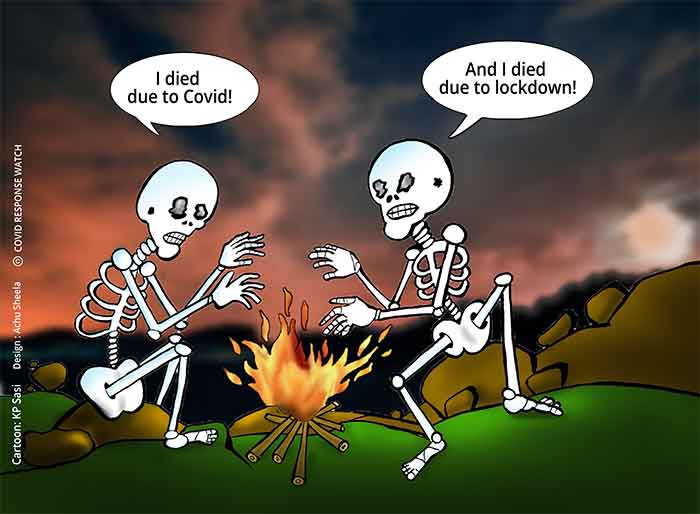
The number of people who have died after contracting coronavirus has also steadily increased during the last six days, but is still significantly below the peak of over 2,000 daily deaths reported in April.
Hospital admission numbers are rising, too. As of Friday, 41,485 people were being treated in hospital, according to the CTP data. This was the highest figure since the end of August, but it was also lower than figures reported in April and July.
Data for Friday has not yet been released by the U.S. Centers for Disease Control (CDC). But on Thursday, the CDC reported 74,380 new cases, its third-highest number on record.
Utah Governor Gary Herbert warned that the virus’s impact had seriously impacted local hospital capacity.
“Up until now, our hospitals have been able to provide good care to all Covid and non-Covid patients who need it. But today we stand on the brink,” said Herbert.
Half a million deaths by the end of February, say experts
The U.S. approach to fight the pandemic and the inconsistent use of masks to prevent virus spread could lead to the cumulative loss of more than half a million lives by the end of February, scientists say.
Researchers from the University of Washington’s School of Medicine predicted that current state strategies surrounding social distancing, phased reopenings and mask mandates could lead to 511,373 deaths by February 28, 2021, according to a study published Friday in the peer-reviewed journal Nature Medicine.
130,000 lives could be saved
Scientists also predicted nearly 130,000 lives could be saved from the end of September through the end of February if at least 95% of the population wore masks in public. If only 85% wore masks, still nearly 96,000 deaths could be prevented.
“We are heading into a very substantial fall-winter surge,” said Christopher Murray, director of the Institute for Health Metrics and Evaluation at the University of Washington’s School of Medicine. “We expect that surge to steadily grow throughout different states, and at the national level continue to increase as we head towards quite high levels of daily death in late December and January.”
The report comes as the U.S. reported record rise in the coronavirus cases with more than 71,000 new cases on Thursday, according to Johns Hopkins University data, marking it as one of the worst days since the height of the summer surge in July.
Dr. Monica Gandhi, a professor of medicine and infectious disease expert at the University of California, San Francisco, said it’s unfortunate that in the U.S. wearing a face mask has become a political or emotional issue rather than a scientific principle.
Change of mind
Minds are not likely to be changed by modeling data forecasts, she said, but they can be a useful tool until enough virologic, epidemiological and ecological evidence is amassed to finally elevate masking is finally elevated to a definitive intervention.
“Short of taking humans, putting a mask on them and then spraying them with SARS-CoV-2, which would be absolutely unfeasible and unethical, this study is very thorough and nicely done,” Gandhi said.
Bob Bednarczyk, assistant professor of global health and epidemiology at Emory University’s Rollins School of Public Health, said Americans may be getting lax as the pandemic drags on.
“Pandemic fatigue is a real thing,” he said. “(This model) is a good reminder of what can happen if we let our guard down and how this can really come back at us really quickly and really forcefully and lead to a lot of death and suffering.”
While model predictions are never perfect, the study’s findings are on track with other recently published data.
A study by researchers at Virginia Commonwealth University in Richmond found the pandemic caused an excess of 225,000 deaths from March to July, suggesting deaths could reach as high as 400,000 by the end of the year as the University of Washington had previously predicted.
Though they may shock the public, Bednarczyk says the projection models should serve as a wake-up call to reinforce the value of masks so death tolls fall short of these numbers.
“People need to start taking this seriously again,” he said. “We want to understand how bad it can possibly get if nothing is done and then we can use that to hopefully work our way back a little bit.”
There is solid data showing that wearing a facemask protects the person wearing it from getting COVID-19 and protects those around them from getting the disease if the wearer is infected.
Public health officials have been calling for Americans to wear masks for months. In July, Centers for Disease Control and Prevention Director Dr. Robert Redfield said, doing so could bring the pandemic to heel in less than two months.
“If we could get everybody to wear a mask right now, I really do think over the next 4-6-8 weeks, I really think we can bring this under control,” he said during an interview with the editor-in-chief of the Journal of the American Medical Association.
Wearing a cloth face covering is estimated to screen out between 65% and 85% of viral particles, said Dr. Chris Beyrer, an epidemiologist at Johns Hopkins Bloomberg School of Public Health.
The fewer viral particles that enter the body, the greater chance the body has to fight them off.
While cloth face coverings are not 100% effective, “wearing those means you’re exposed to less virus. Less is coming in from other people and you’re inhaling less,” said Dr. John Brooks, a medical epidemiologist and the CDC’s chief medical officer for the agency’s COVID-19 response.
The Institute for Health Metrics and Evaluation (IHME), an independent global health research center at the University of Washington, researchers analyzed how the virus spread across states from the first recorded case in the U.S. to Sept. 21. They then used those data to project how adherence to mask use and other variables, such as seasonal pneumonia and testing rates, would impact virus spread from Sept. 22, 2020, to Feb. 28, 2021.
Universal masking—which they defined as 95% of the population wearing masks in public—could save an additional 129,574 lives in that time. If mask compliance dropped to 85%, it would save an 95,814 lives. Without universal masking, more than a half a million lives could be lost due to Covid-19, IHME projected.
Only 49% Americans say they always wear a mask in public.
The IHME researchers said 95% mask use rate in the U.S. is aspirational, but noted that neighborhoods in New York have reached that threshold, while states like Virginia, Florida, and California have achieved 60% adoption of a mask use policy.
The latest data showed the Covid-19 pandemic is nearing its previous high-water mark this summer as a new surge that started in the upper Midwest drifts east to more populous areas. New York’s hospitalizations hit their highest since June.
New York, the early epicenter of the U.S. coronavirus outbreak, reported more than 1,600 new cases on Oct. 22, and 11 additional deaths.
California reported 6,141 new cases Friday, the biggest single-day jump in two months, according to the data from the state health department. The rate of positive tests climbed to 2.8% from 2.6%.
Fauci raises concerns about U.S. surge
Anthony Fauci, director of the U.S. National Institute of Allergy and Infectious Diseases, raised his concerns about the latest surge in U.S. cases. He called it “a precarious place to be” in an interview with MSNBC, saying the cases would lead to an increase in hospitalizations and eventually deaths as the colder weather keeps people indoors.
“We don’t want to shut down the country,” he said. “We’re talking about doubling down on some of the fundamental public health measures,” pointing to universal mask-wearing, social-distancing and avoiding crowds, especially indoors.
He also said the White House task force meetings have slowed to about once a week, and it’s been months since President Trump attended them. A vaccine would likely be available at the end of the year or early 2021, but a more widespread distribution will only be possible months into next year, he said.
Masks for school re-openings
The U.S. Department of Health and Human Services said it is on track to distribute the masks to support school re-openings. “These masks support students, teachers, and staff in public and private schools, with an emphasis on low-income or other high-needs students and schools providing in-person instruction,” the department said.
CDC expands its definition of a COVID-19 ‘close contact’
The U.S. CDC in a new guidance has expanded its definition of a COVID-19 close contact.
The CDC’s latest guidance defines having a close contact with someone infected with COVID-19 as being within six feet of the individual for 15 or more cumulative minutes during a 24 hour period, The Washington Post reports. The CDC previously defined a close contact as being within six feet of an infected person for 15 consecutive minutes.
The new definition, The Associated Press writes, takes into account “briefer but repeated encounters” with an infected person. It specifies the 15 minutes of exposure within six feet is “added together over a 24-hour period,” and so as an example, this could be “three 5-minute exposures for a total of 15 minutes).”
CDC Director Robert Redfield in a statement said “as we get more data and understand this COVID we’re going to continue to incorporate that in our recommendations.” With this change, the Post noted the CDC was “greatly” expanding the group of people considered at risk of contracting COVID-19.
It is easy to accumulate 15 minutes in small increments when you spend all day together — a few minutes at the water cooler, a few minutes in the elevator, and so on,” Johns Hopkins Center for Health Security epidemiologist Caitlin Rivers told The Washington Post. “I expect this will result in many more people being identified as close contacts. This change underscores the importance of vigilant social distancing — even multiple brief interactions can pose a risk.
SIGN UP FOR COUNTERCURRENTS DAILY NEWSLETTER