You guessed it right. I am talking about the dapivirine vaginal ring (DPV-VR), which is one of the top advances happening in the field of microbicides. It is the first long acting prevention product whose Phase-3 randomised controlled studies have shown that using the dapivirine vaginal ring reduced the risk of HIV infection in women and long-term use was well-tolerated.
The World Health Organization (WHO) has just recommended it as a new prevention choice for women at substantial risk of HIV infection as part of combination prevention approaches. The European Medicine Agency has already given a positive scientific opinion on its use, and it has been submitted for regulatory approvals in many countries of Africa and in the USA.
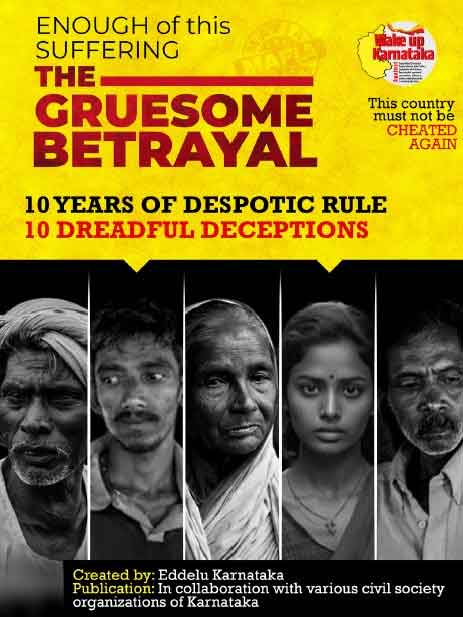
Patriarchal norms have long forced women’s sexual health needs to remain on the blind spot. The economic, social and cultural barriers faced by women often disempower them to exercise their right to negotiate use of prevention options for HIV (and other STIs and unintended pregnancy) with their partners. If we are to end AIDS and achieve zero new HIV infection goal, then it is vital to have more women initiated methods to prevent transmission of all STIs including HIV, and unintended pregnancies. That is why dapivirine vaginal ring provides the much needed ray of hope.
What is the ring?
The dapivirine vaginal ring is a female-initiated option to reduce the risk of HIV infection. It is a silicon ring impregnated with 25mg of the drug dapivirine (a non-nucleoside reverse transcriptase inhibitor). It is easy to bend and insert in the vagina, where it must be worn for a period of 28 days, after which it should be replaced by a new ring. The ring works by releasing the antiretroviral drug dapivirine from the ring into the vagina slowly over a period of 28 days.
This is indeed a revolution in the field of new innovations for HIV prevention, which is now more than just distribution of condoms and pills. And this is just the beginning, with newer technologies in the offing.
“In my own view this is going to be a product that could have real utility because it is extremely safe and because it is such a tiny amount of drug so it would not require a lot of medical monitoring. So it is not going to be very medicalized. All you really need is a rapid test and a dispensation”, said Dr Sharon Hillier, Professor, Department of Obstetrics, Gynaecology & Reproductive Sciences and Microbiology and Molecular Genetics, University of Pittsburgh, during an interaction with a group of select global journalists ahead of the ongoing virtual 4th HIV Research for Prevention (HIVR4P) International Conference.
“When the ring is rolled out, it will be critically important to figure out where to promote it most efficiently. For example, as very little drug comes out of the ring, it might make it a very attractive choice for a woman who is breastfeeding as not much drug will get into the breastmilk. We are doing a study of testing this vaginal ring in breastfeeding women which will be over by September 2021. Another study is also currently underway on pregnant women”, she shared.
Prof Hillier also spoke about next generation rings and approaches to new formulations of delivering drugs for HIV prevention.
The next generation ring (currently under research) has 200mg of dapivirine and can be left in the vagina for 3 months at a time. The first studies, showing that it is safe, have been completed.
Multipurpose prevention technology
There is also a 90 day multipurpose dapivirine vaginal ring currently-under-research that aims to provide dual protection against both HIV and unwanted pregnancy. It contains 200mg of dapivirine and 320mg of levonorgestrel to allow for extended release of the two drugs over 3 months. Results of phase-1 clinical studies, presented at the ongoing fourth HIVR4P Conference, show that it is safe and delivers sustained levels of each drug when used continuously for 90 days- levels likely sufficient to serve its dual purpose for protecting against both HIV and unintended pregnancy. This is going to be a game changer by giving a woman a simple and very safe product in her hands that she can insert in her vagina that could provide both family planning and HIV prevention.
Acceptability and access
There has been great progress in getting HIV prevention products into women’s hands and in having more sustained delivery options. If we create a broad menu of options, people can choose what works best for them, said Prof Hillier. However she concedes that more community education and understanding has to be generated around the utility and use of the dapivirine ring. She said that while a lot of acceptability work has been done in many African countries and in USA, less work has been done in Asia and South America. It was basically designed to address women’s needs in Africa and has been highly acceptable to women there.
Agrees Dr Nyaradzo Mgodi, senior clinical pathologist who is also a part of Scientific Leadership Group of University of Zimbabwe’s Clinical Trials Research Centre, and a lead investigator in Harare for several HIV Prevention Trials Network (HPTN) and Microbicide Trials Network (MTN) studies, including the one on the dapivirine vaginal ring. “This is a very discreet and beautiful intervention, and women, especially in sub-Saharan Africa, like it. It does not interfere with sexual intercourse and does not fall out even when women do manual labour in the fields or lift heavy loads.”
Mgodi is confident that there will be no equity and access issues for delivering the ring even in remote areas of her country Zimbabwe, more so as it does not require cold chain maintenance and has been liked by women once they know how to use it. Her advice is to integrate it with sexual and reproductive health services to speed up its roll-out.
No one silver bullet for preventing HIV
No single prevention product is a silver bullet. There is no single approach that is going to be right for everybody, and at all times. Important insights came from Dr Linda Gail Bekker, Co-Chair of the HIVR4P conference; past President of International AIDS Society (IAS); and Deputy Director of the Desmond Tutu HIV Centre at the Institute of Infectious Disease and Molecular Medicine, University of Cape Town: prevention is relevant only when we actually get it to the people who need it, and they use it. It is not only about the product that works and is available, but also about which product is best for whom, and when is the right time for people to use which product over the course of their lifespan. The bigger is the basket of choices available for HIV prevention, the better it would be.
Shobha Shukla is the award-winning founding Managing Editor and Executive Director of CNS (Citizen News Service) and is a feminist, health and development justice advocate. She is a former senior Physics faculty of prestigious Loreto Convent College and current Coordinator of Asia Pacific Regional Media Network to #endTB & #endtobacco and #beatNCDs (APCAT Media). Follow her on Twitter @shobha1shukla or read her writings here www.bit.ly/ShobhaShukla
shared under Creative Commons (CC)
IF YOU LIKED THE ARTICLE SUPPORT PEOPLE’S JOURNALISM