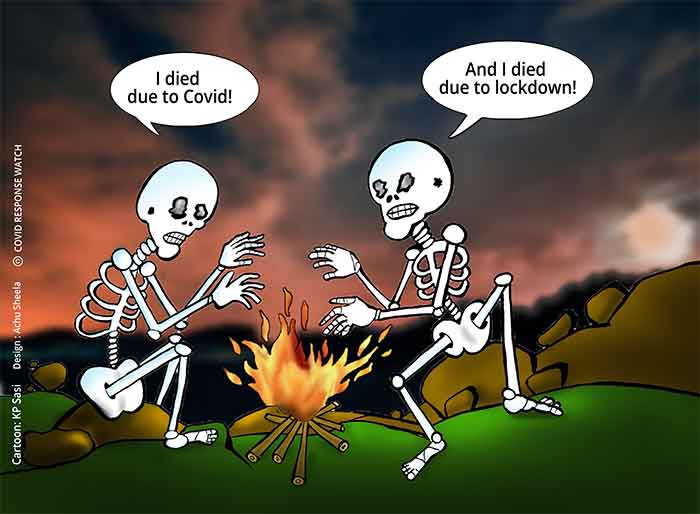
Oxygen ‘audit’ and rationing is taking lives; anesthesiologists say planning adequate buffer stocks is the only way

A string of recent directives, from the central government to states, and from states to government and private hospitals are emphasising on oxygen audits and rationing to ‘prevent wastage,’ as a strategy to ease the oxygen crisis in the country in treatment of Covid-19 patients in the second wave.
But reputed anesthesiologists and clinicians say that rationing orders are ending up forcing them to deny proper treatment to patients.
“In the first wave, we extensively used high flow nasal canula (HFNC) therapy, as we realised that ventilator is not doing any good in the case of Covid. Patients on ventilator are given only about 20 litres per minute (lpm) of oxygen, compared with 50-60 lpm for those on HFNC. With HFNC, we were at least able to save patients from going into ventilator,” explains Dr P C Vijayakumar, chief anesthesiologist & critical care physician and director – academics at Chennai-based Sooriya Hospital.
“But in this wave, we are being forced to do the reverse. We are being told not to use HFNC, to put patients on the ventilator. And even in the ICU, we are trying to accept an oxygen saturation of 90%, whereas it should come up to at least 95%.” Once in the ICU, two in ten patients don’t make it. “Because of the rationing, we are also having to decide which patient has a better chance and provide oxygen accordingly, which is unfortunate. Those who get better after three weeks in the ICU still need oxygen support and are being shifted to non-Covid wards to continue giving them oxygen,” he explains.
Moreover, in this wave, they continue to require oxygen when they go home. With refilling cylinders not being an option (because of shortage), those who can afford it buy oxygen concentrators. But what of the majority who can’t?
“The central government and epidemiologists fooled treating physicians saying that a second wave won’t happen. It did not prepare for more oxygen, beds, medicines, ventilators and concentrators 4-5 months ago and instead was declaring to the world that Indians have natural immunity and have conquered Covid. To cover up for this huge policy failure and unscientific approach, we are now being forced to give inferior treatment in the name of rationing – this is wrong. No government can tell the doctors what to do medically, but when they issue guidelines, it works on us and impinges on our freedom while treating patients,” says Dr Vijayakumar.
Making matters worse is the imposition of an arbitrary formula by the government that projects demand for oxygen in the country based on an ‘estimate’ of requirement per patient per bed, on the treating physicians.
It must be recalled that in September 2020, at the peak of the first wave, doctors objected to confusing notifications and guidelines from central and state governments, setting ‘caps’ on the amount of oxygen to be used per patient. For instance, Maharashtra fixed a limit of merely 7 lpm for non-ICU and 12 lpm for ICU patients, and later on clarified that these were not caps but “assumptions used for planning and forecasting the demand for oxygen.” It also hastened to revise its suggested guidance to 10 lpm (non-ICU) and 40 lpm (ICU), based on the Centre’s September 25, 2020 guidelines to states – the basis of which is also unknown.
Now, it appears, nothing has changed in dealing with the second wave. The affidavit submitted by the Centre to the Supreme Court in the Delhi oxygen crisis, as referred to as recently as in its May 5, 2021 order, further discloses that the expert group comprising Dr V K Paul, member of NITI Aayog, Dr Randeep Guleria, Director, AIIMS, the Director General of ICMR and the Director General of Health Services used a formula for estimating oxygen demand across the country at 24 lpm (100% of ICU beds) and 10 lpm (50% of non-ICU beds) – which is essentially the same used from September last year (24 lpm being an average of the requirement of the three categories mentioned under ‘severe’ cases). Since none of the group’s meeting minutes are in the public domain, it is anybody’s guess how these figures were arrived at. But a number of state governments have issued guidelines, in turn based on such formula, which are being used to ration supply to hospitals, and blindly applied to estimate state-wise demand in this wave too.
One memo by the Government of Haryana dated April 28, 2021, addressed to all deputy commissioners and civil surgeons of the state goes to the extent of saying, “Patient oxygen consumption norms, issued by MoFHW (GOI) shall be followed in letter and spirit.”
Moreover, the Petroleum and Explosives and Safety Organization (PESO), the only organisation handling oxygen supply and logistics, has gag orders from the Ministry of Industry and Commerce on disclosure of any data, says this report.
But behind the shortage of oxygen – and information – what clearly emerges is the central government is playing a cruel joke on doctors and patients. Not only are bureaucrats saying they have made some arbitrary assumptions to ‘estimate’ demand, which will in turn determine how much to produce, and hence, supply, they are also saying, in contradiction, that doctors are free to use any amount of oxygen they deem fit (in Court) and simultaneously issuing guidelines that amount to restricting how much oxygen they can really use!
Instead of attempting real-time demand-supply matching, focus on ensuring buffer stocks of at least five times
A senior anesthesiologist at a reputed government hospital in Chennai feels the government must focus with urgency on creating excess stocks: buffers, not as a fraction of current consumption, but as multiple times that.
“The truth is, the actual extent of oxygen demand simply cannot be extrapolated to what is happening now, which is unprecedented. The requirements of patients are completely unpredictable – a patient who may be alright for six days may suddenly deteriorate and need oxygen on the seventh day, while one ICU patient may be consuming 50% of the entire ward’s requirement. The only thing we can do is to ensure there is a lot of excess oxygen at the hospital level – plan for manifold more, so when the demand shoots up, the supply is available. And if there is less demand, the oxygen will not go waste anyway, it will come into use some time,” she says.
Concurs Dr Vijayakumar, “We don’t know how the government arrives at these figures – calculations cannot and should not be made like that. These ‘guidelines’ can, at most, be taken as a minimum requirement but they are wrongly considering it as the maximum. Instead, the strategy should be to create huge buffer stocks and have supplies handy.”
For instance, Sooriya Hospital has 70 non-ICU and 12 ICU beds in the Covid ward. It has a storage of two liquid oxygen tanks with a combined capacity of about 10,000 litres of compressed liquid oxygen (that would yield about 20 lakh litres of gaseous oxygen). Earlier (in pre-Covid time), they were filled once a day. “Now the requirement is thrice a day but we are able to refill only twice. The shortage is getting worse and refilling even once a day may become difficult if supply does not improve,” he says. The hospital also has a manifold room with 8 cylinders that can be used in emergencies.
A buffer of say, five times the usage, should be made available at all times to meet a sudden surge in demand at the hospital level, he feels.
At the national level, the government needs to immediately prioritise planning for what should be the extent of buffer available in the event of another peak, make available all the raw materials such as zeolite for setting up of pressure swing adsorption (PSA) plants, and increase the number of cylinders available at primary health centres and hospitals in smaller towns (where liquid oxygen is not available) – rather than try a real-time matching of demand and supply, which will fail when demand itself is based on an arbitrary per patient requirement estimation.
Signalling a deteriorating crisis in Tamil Nadu, which has a relatively good public healthcare system compared with most states, the Salem branch of the Indian Medical Association issued a memo out of desperation on May 14 advising private Covid-care hospitals to stop admission of patients due to lack of oxygen, and shift existing patients in the ICU to the Salem GH, demanding the government immediately augment supplies. Against a total requirement of 21 kilolitres/day, it was receiving only 7 kl/day as of May 13, this report reveals.
The turn of events in Kerala, one of the most oxygen-surplus states in the country until late April, that has now been plunged into shortage, also goes to show how unpredictable the course of the pandemic is, and how such demand estimation could go awry, even in the best-managed Indian state in terms of healthcare.
As the National Task Force, convened on the orders of the Supreme Court on May 8, works out its modalities for a “transparent and professional” public health response to the pandemic, it would do well to also pay close heed to what qualified anesthesiologists and treating physicians, who have the real pulse of patient care and Covid treatment, have to say.
(Sowmya is an independent journalist based in Coimbatore)
GET COUNTERCURRENTS DAILY NEWSLETTER STRAIGHT TO YOUR INBOX