Written by Raminder Kaur and Shirin M Rai

Abstract
COVID-19 has revealed deep inequalities in our societies based on class, race, ethnicity, gender, age and region. These inequalities have also been marked by national borders and borderings especially between the global North and South. Orientated between India and the UK, we adopt a mobile and doubly reflexive lens characteristic of a diasporic consciousness to focus on conditions of care and carelessness in the two countries in the face of a global health crisis. We add another lens to the professionalised and the community-based aspects of the “careless society” – that carelessness invokes accidental (careless) as well as a wilful, structural disregard (care-less) that is propounded by the state. Hereon, we denote this conceptual conflation as care/less and examine its articulations in four main overlapping areas: (i) of leaders and the reproduction of privilege; (ii) in undervaluing care labour; (iii) in marginalising people of minority racial or ethnic backgrounds; and (iv) in the lack of investment in social infrastructure.
COVID-19, Care and Carelessness
Dear virus
You are just another silly acronym
To kill us
We already knew how to die
We already knew to end in pyres
End in ashes
End in ditches
End on roads
End on stretchers
End drowned (in us)
Scared alone and
Without love …
There will be many whom we can’’t call again
We have to edit our Facebook friend list
These were people
Who drowned in their own body
(Saif Eqbal, My Friend the Virus, 2021)
March 2020: spring was in the air and so was a new microbe. Shirin came back to the UK from India, where she had been a Visiting Professor in New Delhi’s research institution, ICAS:MP, to the first COVID-19 induced lockdown, empty streets, barely stocked shelves, and to rising statistics of infections and deaths. Raminder cancelled her long-planned trip from UK to India for fear of being stranded by the unpredictability of a fast-evolving global health crisis. Soon, the hospitals were filling up in the UK and stories of health and other key workers under stress as health services struggled to cope were an everyday narrative reproduced endlessly on TV and in social media and the press. Communities particularly affected by this virus were prominent in these narratives – older people, the poor, minority racial and ethnic communities, migrants, and health and key workers. Men too were showing greater vulnerability to the virus, but women were dying in large numbers, nevertheless, because of their overwhelming presence in the health and social care sectors of work. In India, the government was pushing another narrative – of Indian exceptionalism, on the one hand, as Indian figures on infections were presented as relatively low; and of decisive action as a lockdown was imposed without any warning, with catastrophic outcomes for informal workers and the precariat.
COVID-19 has revealed deep inequalities in our societies based on class, race, ethnicity, gender, age and region. These inequalities have also been marked by national borders and borderings – physical, epistemological and political – especially between the global North and South, as vaccines were bought up by the rich countries. Some countries were red-listed as dangerous, and their citizens denied entry to others as nationalist populism filtered through the media. But borders proved futile for pathogens and they continued on their passport-free journeys, mutating as they travelled from place to place, body to body. Whereas the ‘‘UK variant’‘ of the virus denotes a geography of first detection, the ‘‘Indian variant’‘ is overdetermined by ethnicity and connotations of dirt and deterioration as people in India and its diaspora continued to be viewed through a derogatory and racialised lens.
India and the UK remain connected by histories of colonialism, migration, large diasporas, and also by the rise of populist nationalism, neoliberal economic policies, bilateral trade deals, and strategic alliances. Orientated between these two countries, our readings of newsfeeds came from multiple sources and our responses to the pandemic were inevitably comparative. It is this mobile and doubly reflexive lens characteristic of a diasporic consciousness that we adopt in this article to focus on conditions of care and carelessness in the face of a global health crisis.[1]
From who is worse affected by the pandemic to who is able to access good health services, economic support and social care, we find markers of inequality producing devastating material effects. As we witness the deaths of hundreds of thousands of people in this pandemic, we also note the ripple effects of harm – the strains and even collapse of public health systems, the burden on family and community lives and livelihoods as well as the mobilisation of care workers without paying due attention to their health, safety and related needs. Among those who have died, a majority is of the poor, the marginalised and racialised; among those who have cared, a majority is of women. The fabric of our societies seems to be fraying even more under the onslaught of this pandemic, and it seems that those at the bottom of the pyramid are taking most of this burden in a careless global society.
In 1995 John McKnight wrote about the careless society, arguing that it is ‘‘the ability of citizens to care that creates strong communities and able democracies’‘ (ix) and that ‘‘As citizens have seen the professionalized service commodity invade their communities they have grown doubtful of their common capacity to care, and it is that we have become a careless society…’‘ (1995: x). McKnight saw the professionalisation of human services, as he calls them, of medicine, social care and the criminal justice system as a reason for communities become careless. In 2019, Beatrice Muller wrote a different paper on carelessness – ‘‘The Careless Society: Dependency and Care Work in Capitalist Societies’‘ in which she ‘‘analyzes the status of care work in capitalist societies’‘, which results in ‘‘value abjection’‘ of both care work and of those that perform this labour (2019: 1). Now the careless societies referred to in these two pieces of work are fundamentally different – Muller notes the plurality of societies rather than a uniform framing of ‘‘the careless society’‘. McKnight points to professional services as the problem for community-based care, which is the only way that society can collectively care; at no point does he either reflect upon who ‘‘does care’‘ – whose labour is mobilised within the home and in the community to care for others. In rejecting public services, he also overlooks the structures of support for those who ‘‘do care’‘ – the unpaid carers within the home, and within the community, the poorly paid health workers, the undervalued and underinvested in systems of public care, together make for the careless society that Muller speaks of. While we adopt Muller’’s perspective on the careless society, we add another lens to their professionalised and the community-based aspects – that carelessness invokes accidental (careless) as well as a wilful, structural disregard (care-less) that is propounded by the state. Hereon, we will denote this conceptual conflation as care/less.
There are four main overlapping areas to examine in our enquiry on care/lessness in UK and India: (i) of leaders and the reproduction of privilege; (ii) in undervaluing care labour; (iii) in marginalising people of minority racial or ethnic backgrounds; and (iv) in the lack of investment in social infrastructure.
- Care/lessness of leaders and the reproduction of privilege
Right-wing leaders – of which prime ministers Boris Johnson and Narendra Modi are mutating variants – took notice of an impending public health crisis, but they denied and repudiated the seriousness of the claims as well as the scope of the spread. With their crowd-pleasing and devil-may-care braggadocio, they fooled themselves as well as most of their publics into thinking that the virus will remain contained to other countries even if it had exited China and shown its capacity to spread widely and quickly from one to another epicentre (Ahmad 2020). The language of nationalism with its shades of xenophobia soon got attached to this spread – there was the original Chinese variant, the Brazilian variant, the South African variant, the Kent (in the UK) variant and now the Indian variant.
In the UK. reports from anonymised officials revealed how emergency COBR (Cabinet Office Briefing Rooms) meetings were ‘‘disasters’‘ as the government was ill-prepared for a pandemic believing that COVID-19 was no worse than flu. ‘‘The government machine was breaking in our hands’‘ reported one official and that the ‘‘conversations were totally in the wrong universe’‘. [2] Internal reports from Indian officials are not in the public arena, due to severe punitive measures against the press and officers in the country. However, the observation that ‘‘we were more blind than we told the public’‘ would be equally relevant to the Indian administration.[3] Indeed, even after leaders’‘ eyes were opened to the fast and furious pace of the virus, lessons were not learnt as has come glaringly to light in the tsunami second waves in both countries. Dr J.A. Jayalal, national president of the Indian Medical Association, observed healthcare was not a priority compared to the economy, made worse by the fact that ‘‘Budgetary allocation for health hasn’t gone beyond 1.2-1.5% of the GDP in India when countries such as the U.S. and the UK spend 16% of GDP on public health’‘ (Bhaya 2021).
Initially, Johnson evangelised about the unproven doctrine of ‘‘herd immunity’‘ where, it was believed that over time, a significant percentage of the population would develop biological resilience if not resistance to the virus (Kaur 2020) – an official recalled how they discussed ‘‘Chicken pox parties to help the virus spread among the healthy population’‘.[4] The Conservative party administration emphasised the resilience of national stock and, failing that, scientific investment and genius in developing the vaccine. In the face of growing scientific evidence and the rapidly rising infection rates, the government imposed the first lockdown on March 16, 2020 along with emergency police powers and penalties now under review by a cross-parliamentary Joint Committee on Human Rights after their alleged illegality.[5]
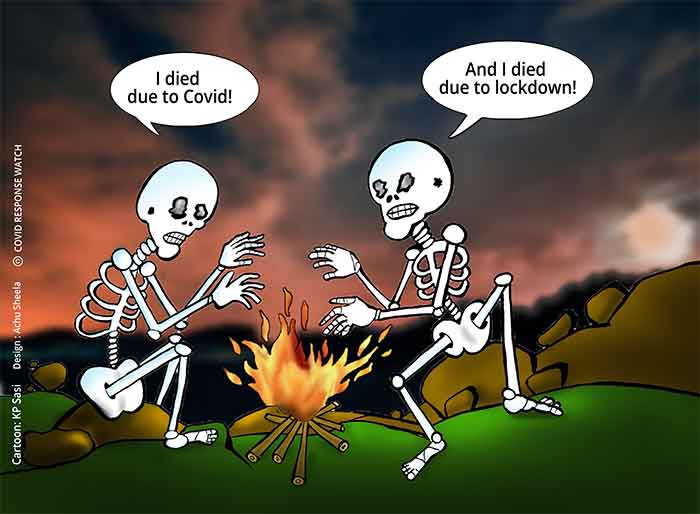
In India, Modi enforced a sudden lockdown on March 26, which left millions unprepared and thousands of informal workers out of jobs and homes. Under the cover of this lockdown, there was also initiated a political crackdown as non-violent protesters against the government’s constitutional amendment from December 2019 were arrested and their campaign brutally suppressed in March 2020 (Rai, 2020). Arrests were largely against those from poor and minority communities (Bej et al. 2020). Migrant labourers – informal and domestic workers – were thrown out of their jobs and, without any government support were forced to walk hundreds of miles to return to their villages; hundreds died (Roy 2020). State support especially from central government was non-existent, and was met, to the extents possible, through grassroots efforts of trade unions, non-governmental organisations (NGOs), charities and gurdwaras (Sikh temples) who stepped up to supply the needy with basic sustenance.
Lockdown was lifted as carelessly as it was imposed in both countries. In the UK, a rush to get the economy moving after the first lockdown made for a perfect storm over the winter when the virus was most likely to spread. With Conservative campaigns to get people ‘‘to eat out to help out’‘ over the summer, the opening up of schools and movement of students to universities in the autumn, and lifting of lockdown for Christmas in winter, the virus had full reign and led to a soaring daily death rate.
By March 2021, after months of denial, patriotic triumphalism declaring victory over the virus in India, and the zeal for large election rallies and religious celebrations led to massive government sanctioned gatherings where, a double mutant variant of the virus became rampant. As infection rates spiked, people literally did not have enough oxygen to help them breath. On the one hand, grassroots initiatives and social networks worked to provide compressed oxygen cylinders to desperate families. On the other, a black market thrived in response to people’s pleas for oxygen, pleas that were penalised by the Bharatiya Janata Party (BJP) government, in the name of stopping spreading rumours and ‘‘misleading information’‘ – in one case leading to the arrest of a man concerned about his grandfather.[6] Even while the national and international community poured funds and health provisions to alleviate the thousands of daily fatalities, a slow bureaucracy burdened with red-tape and laws such as the Foreign Contribution (Regulation) Act (FCRA) meant that they could not swiftly access the provisions to come to people’s aid. In the meantime, more and more people died for a lack of oxygen, a lack of care.
The pandemic created a struggle not simply for the survival of the fittest but the survival of the richest. The herd in ‘‘herd immunity’‘ is an allusion to a privileged stock of grazing ungulates. In both countries, elites were left relatively unscathed. While several of the middle classes were able to carve out offices in their homes to continue to teach, manage, administer and/or create, keyworkers were compelled to work in relatively close contact with others without adequate protection. They were the ones who could not afford to disconnect. UK’s Chancellor Rishi Sunak might have delivered a package of economic care for those who could not work, businesses and charities still found it hard or a long-drawn out process to access the funds. While opportunities and supplies were cut short, bills were not and many plunged into debt if not unemployment itself. And with an inadequate welfare or universal credit system, many lived in fuel poverty and became reliant on the charity of food banks. Young people out of schools, colleges and universities in particular were left with a bleak future – a scenario that compounded mental health issues with little recourse to support services (British Academy 2021). The true extent of the COVID costs to health and wellbeing are yet to be fully gauged.
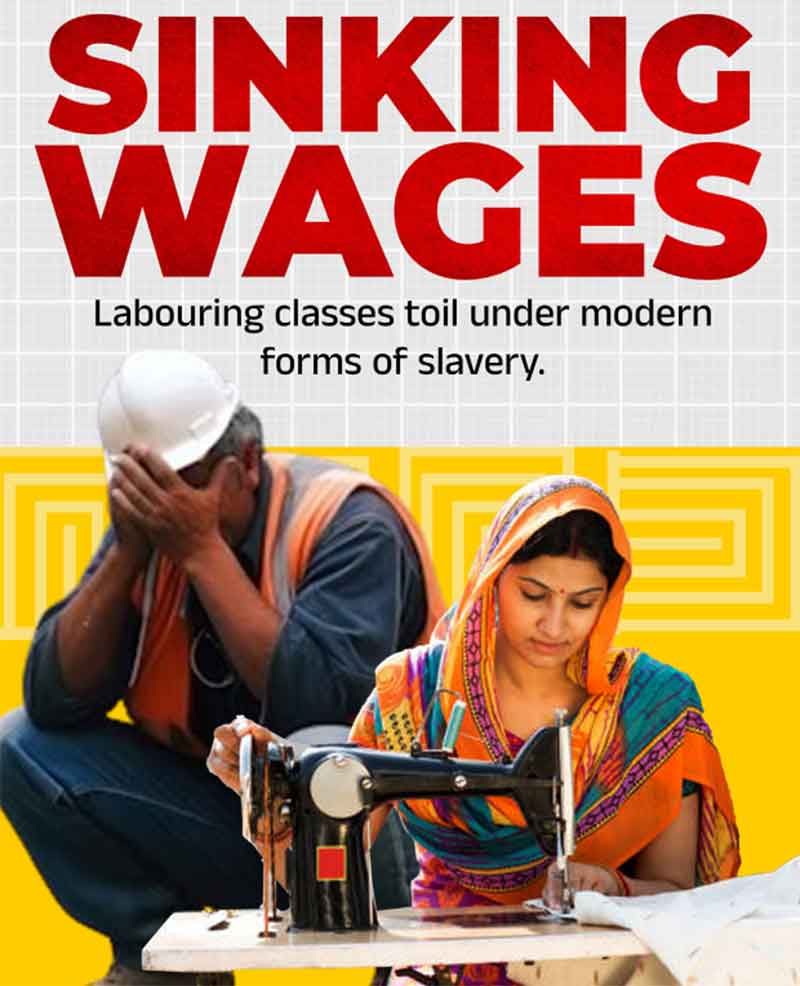
- Care/lessness in undervaluing care labour
Rajagopal et al (2020) note that in UK, ‘‘Of the NHS staff who have sadly died from Covid-19, 63% were from BAME background. This included 71% of the nurses and midwives, 94% of doctors and dentists, 56% of the healthcare support staff and 29% of other healthcare personnel, who died’‘. According to Skills For Care, UK’s Black and Asian Minority Ethnic (BAME) communities account for 1 in 5 of the social care workforce in England (2020); given the above statistics for BAME vulnerability to COVID-19, the shortage of PPE for social care staff in the first few months of the pandemic and high incidence of spread of infection in the social care sector, BAME carers have been particularly vulnerable. Further, as households cope with the pandemic, the care work within the household, which is also profoundly gendered, has increased, putting enormous pressure on women in BAME communities. Fawcett Society notes that 45% of BAME women said they were struggling to cope with the different demands on their time; it is not surprising then that life satisfaction and happiness were lowest for BAME women (2020). Women’s Budget Group found that ‘‘Close to half (42.9%) of BAME women expect to struggle to make ends meet in the coming months and to be in more debt than before the pandemic. A quarter of BAME mothers are struggling to feed their children’‘ (2020:7).
In India, 17 million women lost their jobs in April 2020, raising unemployment among women by 15% from a pre-lockdown level of 18%. These women are also 23.5% less likely to be re-employed compared to men in the post-lockdown phase (Dutta 2021). The Institute of Social Studies Trust (2021) found that among those who could retain their jobs, around 83% of women workers faced a severe drop in income, 66% experienced an increase in unpaid care work, even though middle-class women were better able to cope by buying in labour of other women. [7]
Health and key workers have taken a heavy toll of death and illness during COVID-19. In more rural and remote areas in India, trained staff are hard to come by (Chaurasia and Ellis-Petersen 2021). In the cities, medical staff are bombarded by an increasing number of patients and decreasing amounts of supplies. The mental and physical toll has led to the death of over 860 staff since the pandemic began including the depression and suicide of younger doctors who are thrown in at the deep end without adequate training or support (Bhaya 2021). Undoubtedly, while the varying pictures in UK and India owe to the care/lessness of colonial legacies, they converge when they promote a neoliberal philosophy and political economy that opens up health infrastructures to the cruelties of cannibalising capitalism, a theme that we return to below in the last section of the article.
- Care/lessness in marginalising communities of difference
Much before the pandemic hit, the Commission on Care (of which Shirin was member) found that local authorities often labelled BAME groups as ‘‘hard to reach’‘ and therefore overlooked them in their work; it cautioned against assuming that in BAME communities ‘‘folk look after their own’‘; it also found that the short-term nature of funding for projects specifically targeting BAME groups meant that long term issues were not addressed’‘ (2016: 16). Finally, language barriers mean that BAME groups report greater difficulties in getting information they need (Gunaratnam 2007). This also means that they are less well-integrated into the wider community that may have better access to information (Commission on Care, 2016: 17).
In India, Dalits and tribal communities were overlooked in the treatment for disease or vaccinations.[8] The poor, always inflected by caste politics, also suffer. While accurate statistics are scarce, researchers affiliated with Stranded Workers Action Network (SWAN) report 972 deaths between March and July 2020 who died from starvation, exhaustion, financial distress, road or train accidents, suicide, police brutality and a lack of medical care. Other reports by Action Aid India and the Centre for Sustainable Employment paint a picture of dire destitution noting that the majority of workers who they surveyed had lost their livelihoods and incomes with no other support to rely upon other than meagre rations and the good will of individuals and grassroots collectives (Mohanty 2020).
‘‘Misinfodemics’‘ allied with hate crimes against minority communities has compounded the problem (Mukhtar 2021, Yasmin 2021). In India, COVID-19 culpability was cast against large gatherings for the Islamic missionary movement, Tablighi Samat, along with the Sikh-dominated farmers’‘ protests against 2020 legislation (kale kanoon or black laws) in a context of rising Hindu nationalism (Kaur and dyuti a. 2020, Saini 2021). In the UK, racist attacks against Chinese and East Asians went up by 300%, according to End the Virus of Racism, a UK-based advocacy group (Khan 2021). UK’‘s hate crime monitoring group, Tell MAMA, reported a 40% increase in cases of online Islamophobia during the first lockdown. ‘‘White communities are starting to see Covid as a ‘‘brown problem’‘ reflected Zulfi Karim, the deputy lieutenant of West Yorkshire (cited in Pidd et al 2020). In both countries, Islamophobia and casteism or racism then reveal the lie of the prevalent rhetoric of ‘‘we’re all in it together’‘.
- Care/lessness in not investing in social infrastructure
When it comes to the professionalised care services, health systems have either been neglected or stripped of their value through extractive outsourced contracts in a neoliberal world. The British Medical Journal (2021) reported: ‘‘Over 850 UK healthcare workers are thought to have died of covid [sic] between March and December 2020’‘ and many more fell ill. The underinvestment in care and health sectors has ensured this high cost of care/lessness – the Union health budget in India is about 0.34% of GDP; while the figure for the UK is much higher, at 7%, the Health Foundation reported that ‘‘Health spending as a share of GDP remains at lowest level in a decade’‘ (Jones 2014; see also Sekelala 2020). In UK, the Conservative administration’s thin veneer of appreciation for the NHS rubbed off when the Chancellor’s 2021 Spring budget revealed that NHS staff would receive no more than a 1% pay rise – now under review after widespread criticism (Walker et al. 2021). Due to the generally egalitarian approach adopted by NHS staff, treatment and vaccination programs have remained transparent and fair, even though questions have been raised about racism and frontline work allocation in the system.
While care/lessness is manifested in the lack of regard for the health of the poor, we cannot overlook the systematic privatisation of health care over the last couple of decades in both countries. The state-supported healthcare in India is the last port of call for anyone poor in dire health straits but is woefully underfunded and stands more as a decaying carcass than a sufficiently-staffed and well-sourced infrastructure. Those who have the means rely upon health insurance and savings to access a private hospital – with their varying menu of services and costs that go up due to demands in a health emergency (Thiagarajan 2020). While efforts to apply caps to bills have been initiated, a lack of enforcement means that cases of COVID-19 might still bankrupt the family.
Transnational lifelines
A comparative overview of care/lessness in two countries corresponds to a diasporic consciousness that traverses locality and globality: concern for the self, family and friends, that need navigate national strictures as it spans continents. The analysis of care/lessness in the two countries reveals several points of divergence and convergence. It goes without saying that the two nations represent varying sides of the inequities between the global North and South in terms of representations, resources and infrastructures. But India is an emerging economy next to the faltering economy of a broken Britain, and there are strands that bring them together: the privilege afforded to the political and economic elites in each country, the disregard for women, health and careworkers, migrants and people of different races or ethnicities to the majoritarian populace, and leaders that call upon a disingenuous populism reliant upon a complex of religion, race and nationalism. National sovereignty too provides convenient alibis to paper over cracks in the system. Such strategies of distraction where elites pertain to be a part of the people while living in luxury and spacious dwellings have a wider purview than the two countries here alone.
As India seeks to be a regional superpower, it has neglected basic provisions for its more vulnerable and marginalised populations. Similarly, while post-Brexit Britain seeks to carve out a new position of hegemony after its departure from the European Union, it does so with scant regard for those considered at the bottom of the racial, gendered and economic pyramid. Leaders might continue in their virtual summit to seal deals and discuss strategies, but for lesser mortals – as underlined by the opening poem – virtual media is a lifeline for appeals for oxygen and confirmation that loved ones are still breathing.
References
Ahmad, Talmiz. 2020. “Self-Absorbed, Uncaring, Incompetent: COVID Has Exposed Populist Leaders for What They Are’‘. June 29. https://thewire.in/politics/trump-bolsonaro-jognson-modi-populist-leaders-covid
Bej, Srujana, Nikita Sonavane and Ameya Bokil. 2020. ‘‘Arbitrary & Disproportionate Criminalisation of Marginalised Communities: A Countermap of Pandemic Policing in India”. Oxford Human Rights Hub. ohrh.law.ox.ac.uk/arbitrary-disproportionate-criminalisation-of-marginalised-communities-a-countermap-of-pandemic-policing-in-india/
Bhaya, Abhishe.k 2021.’‘India’‘s COVID-19 crisis: 116 medics dead in 25 days; 860 since the pandemic began’‘. CGTN May 7. news.cgtn.com/news/2021-05-06/India-loses-116-medics-in-25-days-amid-raging-second-COVID-19-wave-102HwmAvffq/index.html
British Academy 2021. The COVID decade: Understanding the long-term societal impacts of COVID-19. www.thebritishacademy.ac.uk/documents/3238/COVID-decade-understanding-long-term-societal-impacts-COVID-19.pdf
Chaurasia, Manoj and Hannah Ellis-Petersen. 2021. ‘‘Covid rips through rural India’‘s threadbare healthcare system’‘. The Guardian May 7. www.theguardian.com/world/2021/may/07/covid-rips-through-rural-indias-threadbare-healthcare-system
Dutta, Diya, 2021. ‘‘How the post-pandemic world can be more equal for women’‘. Forbes India https://www.forbesindia.com/article/12th-anniversary-special/how-the-postpandemic-world-can-be-more-equal-for-women-by-diya-dutta/67987/1?fbclid=IwAR3cTmA30Q8eggnMwB6hsEcrJFh47pTYfeOA5Dc9CGmHh4XLUiN0NTW-Gb8
Institute for Social Science Trust, Women and Unpaid Work https://www.isstindia.org/publications/1615809448_pub_1_Women-and-Unpaid-Work_-_IWWAGE.pdf
Jones, Owen. 2014. The establishment: And how they get away with it. Harmondsworth: Penguin.
Kaur, Raminder. 2020. ‘‘Amidst backward-walking somnambulists.’‘ HAU: Journal of Ethnographic Theory. 11(1): 339-344.
Kaur, Raminder and dyuti a. 2020. ‘‘Reclaiming the sublime: The (un)making of the people’‘s constitution in India.’‘ HAU: Journal of Ethnographic Theory. 11(1)
Khan, Aina. 2021. ‘‘I don’’t feel safe’‘: Asians in the UK reflect on a year of hatred’‘. Al Jazeera March 23. https://www.aljazeera.com/news/2021/3/23/i-dont-feel-safe-asians-in-the-uk-reflect-on-a-year-of-hatred
Mohanty, Basant Kumar. 2020 ‘‘Migrant deaths government won‘t see.’‘ Telegraph India September 16 www.telegraphindia.com/india/coronavirus-lockdown-migrant-deaths-govt-wont-see/cid/1792114
Mukhtar, Sonia 2021. ‘‘Psychology and politics of COVID-19 misinfodemics: Why and how do people believe in misinfodemics?’‘ International Sociology. 36(1): 111-123.
Pidd, Helen, Josh Halliday, Amy Walker and Nazia Parveen 2020. ‘‘Islamaphobia surges amid lockdown warn civic leaders in north of England’‘. The Guardian August 5
Rai, Shirin M, 2020. ‘‘India: from populist nationalism to popular constitutionalism’‘.OpenDemocracy, https://www.opendemocracy.net/en/openindia/india-populist-nationalism-popular-constitutionalism/
Rajagopal, Manoj, Radhika Kaimal, Sunil Nedungayil, 2020. ‘‘BAME healthcare workers and Covid-19’‘ https://www.gmjournal.co.uk/bame-healthcare-workers-and-covid-19
Roy, Arundhati. 2020. ‘‘The pandemic is a portal’‘. Financial Times. April 3 www.ft.com/content/10d8f5e8-74eb-11ea-95fe-fcd274e920ca
Saini, Ravinder 2021. ‘‘Poor infra to blame for surge, not us: Farmers’‘. The Tribune. May 15. www.tribuneindia.com/news/haryana/poor-infra-to-blame-for-surge-not-us-farmers-252896
The BMJ Opinion, 2021. ‘‘Up the line to death: covid-19 has revealed a mortal betrayal of the world’‘s healthcare workers.’‘ https://blogs.bmj.com/bmj/2021/01/29/up-the-line-to-death-covid-19-has-revealed-a-mortal-betrayal-of-the-worlds-healthcare-workers/
The Wire, 2021. ‘‘Health spending as a share of GDP remains at lowest level in a decade’‘ https://www.health.org.uk/news-and-comment/charts-and-infographics/health-spending-as-a-share-of-gdp-remains-at-lowest-level-in?gclid=Cj0KCQjw7pKFBhDUARIsAFUoMDZOjIg5unNLnDKcD8svsAxoxOhCP34
iHRfGVcvLLUC1NxNVzywE6O4aAnrhEALw_wcB
Sekelala, Sharifah, 2020. ’‘Healthcare workers “at the frontline” of COVID–19.
https://blogs.warwick.ac.uk/po901/entry/healthcare_workers_at/
Thiagarajan Kamala 2020. ’‘Covid-19 exposes the high cost of India’‘s reliance on private healthcare’‘ BMJ 370 :m3506 doi:10.1136/bmj.m3506
Walker, Peter, Aubrey Allegretti and Ben Quinn 2021. ‘‘Anger grows at offer of 1% pay rise for NHS staff.’‘ The Guardian. March 6www.theguardian.com/society/2021/mar/05/anger-grows-at-offer-of-1-pay-rise-for-nhs-staff
Yasmin, Seema 2021. Viral BS: Medical myths and why we fall for them. Baltimore: John Hopkins University Press.
[1] This article is part of our ongoing ESRC-funded research as part of the Consortium on Practices of Wellbeing and Research among Black, Asian and Minority Ethnic Families and Communities (Co-POWeR).
[2] These quotes are from the documentary, COVID confidential with Laura Kuenssberg (2021), the political editor of BBC News.
[3] Covid confidential with Laura Kuenssberg (2021).
[4] Covid confidential with Laura Kuenssberg (2021).
[5] committees.parliament.uk/committee/93/human-rights-joint-committee/news/154842/joint-committee-on-human-rights-every-fixed-penalty-notice-issued-under-coronavirus-regulations-must-be-reviewed/
[6] www.bbc.co.uk/news/world-asia-india-56894757
[7] Women, Work and COVID-19: Enterprises, SHGs and Workers | Economic and Political Weekly (epw.in) www.epw.in/engage
[8] Suraj Telenge in Covid India public meeting organised by Warwick University and SOAS. May 18, 2021.
Raminder Kaur is based in the School of Global Studies at the University of Sussex and author of several books and articles, the latest of which is Kudankulam: The Story of an Indo-Russian Nuclear Power Station (OUP 2020).
Shirin M Rai is professor in the Department of Politics and International Studies and the Director of Warwick Interdisciplinary Centre for International Development. Her latest books are Performing Representation: Women MPs in the Indian Parliament, Oxford University Press, 2019 and the Handbook of Politics and Performance (co-edited), Oxford University Press, 2021.
GET COUNTERCURRENTS DAILY NEWSLETTER STRAIGHT TO YOUR INBOX