Writing in his book “Late Victorian Holocausts: El Niño Famines and the Making of the Third World”, Mike Davis describes the Anti-Charitable Contributions Act of 1877, introduced in India when it was being ravaged by a famine, by then Viceroy Lord Lytton which “prohibited at the pain of imprisonment private relief donations that potentially interfered with the market-fixing of grain prices.” In Davis’ accounting of colonial horrors wedded with “liberal” dogma, Lord Lytton’s diktat against charitable contributions stands out for its alarming cruelty.
In thinking of similarly cruel analogs in today’s neo-liberal era, it is hard to look past Intellectual Property (IP) laws (these laws are trade barriers, and establish that “liberalism”, neither old nor neo, was ever about “free trade”.) For instance, when medical technology considerably mitigated the risk of AIDS, it took almost a decade before countries in the global South like South Africa, could benefit from them. This was not because of any fundamental factors around the cost of production or distribution of the AIDS drugs, but because of patent monopolies, monopolies that could have been suspended or ended at the stroke of a pen. Similar examples abound, e.g. with the price of insulin, the price of drugs treating cystic fibrosis and tuberculosis, illustrating the global significance of this issue. As with the justification for the Anti-Charitable Contributions Act, the justifications offered for IP laws, namely that it is necessary to sustain medical innovation, appear as sincere as the statutory warnings issued by nicotine peddlers.
For instance, India was prevented from manufacturing generic medicines for cystic fibrosis because of a patent under Indian law, using which the patent holder sold a whopping nine units in the Indian market.
The above topic has come into sharp focus due to the pandemic, in the context of access to vaccines, with rich countries backed by big pharma blocking IP waivers at the WTO, and leading to calls to look towards China and Russia. In order to trace the history of these IP laws through the neoliberal period, I sought out Achal Prabhala who has spent many years of his life focused on these issues. Achal is a fellow at the Shuttleworth Foundation and the coordinator of the AccessIBSA project, which campaigns for access to medicines broadly in the global South, specifically India, Brazil and South Africa.
The interview is divided into three parts. We first discuss the history and impact of TRIPS (The Agreement on Trade-Related Aspects of Intellectual Property Rights), a key arm of the World Trade Organization (WTO) through which the IP regime was globalized. We then discuss the Indian Patent Law of 2005, which is an interesting illustration both of the nefarious impact of TRIPS as well as the resistance to TRIPS. Finally, we discuss covid vaccines and the outsized role that IP laws play in it. Throughout the interview, we observe not only the brutality of the IP regime, but also the currents of resistance to it.
History of TRIPS and its impact, specifically on AIDS treatment
Q: Let us begin by briefly discussing the history of TRIPS, the IP regime of the WTO, which basically forced all member countries of the WTO to institute IP protection laws to be compliant.
AP: TRIPS came into effect as part of the WTO in 1995. TRIPS is binding, and any violation can be taken up in a dispute resolution mechanism; and it has consequences. A violation of TRIPS would mean that the entire ability of a country to trade in the world would be compromised.
Historian Susan K. Sell has written about the background of TRIPS in very interesting detail. Behind the scenes, two companies, IBM and Pfizer, representing tech and pharma respectively, understood by the 1990s that the most efficient way by which they could guarantee global rents, which were already lucrative for them in rich countries, that they could multiply these rents dramatically without doing much more work, was by creating a binding global framework from which countries could not wriggle out of. Prior to 1995, it was a loose framework. Before the WTO, there were various pacts and treaties on IP, but none as comprehensive and binding, and part of a crucial institution like the WTO. TRIPS was an act of (evil) genius on the part of Pfizer and IBM. Once this rule was instituted, it effectively created a compulsory global regime for IP, thus enabling a permanent, binding collection of rent from around the world.
The funny thing with the original TRIPS is that it was never designed as a way to alter the situation in these countries’ primary market. If you look at the global pharmaceutical industry, for instance, for all the talk of India, which is the largest volume generator of generic pharmaceuticals, the contribution of India by revenue, by actual hard dollars is less than 1% of the global Western pharmaceutical pie. India is a low income country. Any gain in volume is beset by the fact that people are paying low prices. When you throw in the value of the rupee vs the dollar, it adds up to a very small quantity in revenue terms. This is paradoxical, and doesn’t square up with the undue attention that the EU and the US pay to things like the Indian patent law. But the reason that the pharmaceutical industry is so interested in India is that it could set precedents that upset the revenue that they earn from their primary markets; precedents that could create dramatically lower prices and that would then create a genuinely crippling problem for these pharmaceutical companies.
The thing with TRIPS is even many neoliberals don’t agree with it, e.g. economist Jagdish Bhagwati who has been a vocal critic of TRIPS from a free-trade, conservative point of view, which should indicate the broad support that the work that people like I do have, across the ideological spectrum. TRIPS is widely despised, except for the technology and the pharma industries that benefit tremendously from it.
Q: Let’s now discuss one of the earliest issues that shed light on the impact of TRIPS, and led to the by now global movement against IP laws, namely AIDS.
AP: Three things happened in the late 1990s. First, it became clear that HIV AIDS was a much more significant problem outside Europe-America than within. The second of course is the creation of the WTO, with TRIPS, in 1995. There’s a third thing that happened in 1996. Western pharmaceutical companies created effective treatments for AIDS. By then, the medical consensus was that an effective antiretroviral cocktail (called HAART – Highly Active Antiretroviral Therapy) would be able to sufficiently treat HIV/AIDS. That is the medical breakthrough of 1996. These treatments changed AIDS from a death sentence to a chronic condition; they were like the discovery that insulin could treat diabetes.
This medication cost $10000 per person per year, which back then, was an impossible sum of money for anyone in India or S. Africa to think about paying even for their own lives. In 1998 in South Africa, the Treatment Action Campaign was formed. This was a group of people who were
HIV-positive who said, we may be poor, we may be LGBTQ, completely marginal, but we’re HIV positive and we’re not going to die. Of course, many of them did. The solution wasn’t instant.
But when they started working for accessible, affordable AIDS treatment in S Africa in 1998-1999, it struck a chord around the world.
In 2001, the head of Cipla, a generics manufacturer in India was visited by a group of American AIDS activists. They said we have these drugs that are highly effective, but we just can’t use them because they are too expensive. They brought with them activists from Doctors without Borders. MSF was running a clinic in S. Africa where they were trying to treat HIV/AIDS. Even MSF could not afford the $10000 per person per year that was required. The Cipla owner said I can make these drugs for you at $350 a year, less than 30 times the original cost. That made instant international headlines. Incidentally, many Indian activists understood the solutions that were available to them. And the global importance of securing the Indian generic pharmaceutical industry. Not just for what it could do for India, but for every developing country in the world. Back then, we had a capacity for pharmaceutical production that no other developing country had. We still do, but it’s more broadened.
By the time S. Africa could set up affordable treatments, it was 2004-5. Availability of generics in India didn’t mean availability in S. Africa at the same price. In fact, S. Africa understood this and changed its laws in 1997 to import generics to fight AIDS. It was immediately sued not just by a consortium of western US pharmaceuticals, but also supported by the US government. Al Gore as Vice President specifically intervened in that case to support the suit against S. Africa, to prevent S. Africa from making the most minor modifications to see if it could import AIDS drugs at an affordable price. The case ran for about 2 years and then was dropped under mounting public pressure from activists in S Africa and activists in the US, at a time when Al Gore was no longer VP, but running for President. So S. Africa faced obstacles at every step in its attempt to access medicines for HIV/AIDS, and it took a few years for the blocks to be cleared up.
The Indian Patent Law of 2005
Q: Let us discuss the Indian patent law of 2005. In order to be TRIPS-compliant, India was forced to support product patents (whereas its previous patent law only covered processes, not products.) Nonetheless, within the framework of TRIPS and WTO, you describe it as an example of resistance. Can you explain why?
AP: There is this expansion in the idea of intellectual property as a clever 21st century way of doing business. In the pharmaceutical space, the biggest shift is to move away from primary compound patents which are patents that cover newness, e.g. a new chemical entity that has come to market, to patents that cover trivial modifications to that new chemical entity, that aren’t new in any commonsensical way or in any medical or legal sense. The idea roughly is this: you invent a new chemical entity and it’s in the form of a pill. You could also liquidize that and that has its own set of patent protections. Sometimes you can tinker with the method of delivery.
Sometimes you can add something to the entity that doesn’t change the entity itself. All of these trivial modifications would receive patent protection. From a logical point of view, you would think you could have one primary compound patent covering one chemical entity. Instead, you would have these estates, with perhaps a primary compound patent at the core, but around it, literally 100s of trivial patents. What that meant is there was a standard idea of what patent law should look like and that was driven very much by what was done in the US and Europe, which in turn was driven by what the pharmaceutical industries in those countries wanted.
In 2005, India created a different idea of a patent law with a much higher bar for innovation. Several countries have done small things to express their discontent at this Euro-American version, but India rebelled most articulately. The way it did was to disallow patents for trivial modifications: you cannot get a patent to turn a powder into a liquid. Any modification of a chemical entity can only be protected by a new set of monopolies if you can show that clinical and therapeutic efficacy of the new chemical entity has substantially changed. That was the principle that drove Indian patent law in 2005. It was a huge change and went against the normal manner of patenting in some of the richest countries in the world who felt affronted by it, not because they were going to miss out on revenue in India, but because they were worried that other people might get the same idea.
Q: Can you describe the history behind the Indian Patent Law of 2005?
AP: In 1947, at the time of independence, India had a colonial patent law. Post-independence, in the era of import substitution, India took seriously the complaints of the indigenous pharmaceutical manufacturers that these patent laws were getting in their way of making drugs that were needed in a manner that would be affordable and accessible to people. In response, in 1970, a new patent law came into force. The 1970s and 80s were a period that you could call the golden age of the Indian generic pharmaceutical industry. They were allowed to grow within the country. These were industries that were primarily serving India and did so very well, because they only had to reverse-engineer. There wasn’t a whole lot of innovation in coming up with new compounds, but there was innovation in coming up with looking at safe and effective ways of re-creating helpful chemical compounds in India, and also creating the legislation and regulation to ensure that those were safe. They put them out, they grew and became capitalized, multi-billion dollar industries very early on.
In the 1990s, as the world moved towards creating the WTO, it wasn’t clear to India how affected they were going to be by TRIPS. In hindsight, you could say they should have done more to oppose WTO. But my understanding from speaking to government negotiators who were involved in the multilateral talks at the time is that the implications of TRIPS were just not understood.
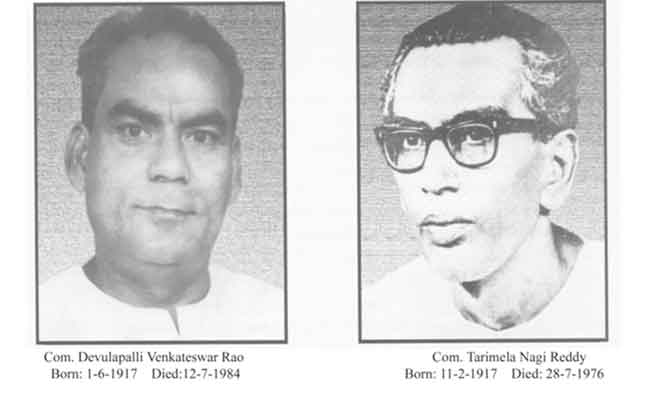
Then we had the advent of AIDS, after which the implications of TRIPS became very clear. According to the 1995 WTO terms, India had, as a developing country, until 2005 to get its patent law in order. Until then, India could operate under the existing patent law with very few changes. But activists and researchers, and even politicians understood that that holiday was coming to an end in 2005. The 2004 elections brought Congress to power, but their power was dependent on the support of the Left parties specifically CPI(M). So, the left parties could extract a larger share of policy decisions. One of the policies where they asserted themselves was the patent law. In the run up to 2005, towards the end of 2004, the Congress had literally just won, a leaked draft of the patent amendment terrified activists including me (I wrote about it at the time) because it was literally the same draft as had been developed by the previous right-wing BJP government. The BJP draft would have delighted first world countries. So there was an outcry around this. The communist parties got involved with it. They intervened to ensure that a different draft was promulgated eventually. So, it’s because of a remarkable confluence of circumstances that have never repeated themselves that we have the law that we do.
Q: Let us discuss the impact of the above law.
AP: India needed some time to institute offices and a regime that could execute, and so India only started examining patents in 2009. It took 4 years to create a system that could implement the law. What happened between 2005 and 2013 was that Novartis, a Swiss-American pharmaceutical company was protesting the denial of a patent to a form of a drug called imatinib, which they marketed as Gleevec, for Chronic Myeloid Leukemia, a form of blood cancer. Their protest against the Indian government took two forms. The first was a constitutional challenge. They launched it at the Madras High Court in 2007, and argued that Section 3d of the Indian patent law of 2005 was used to deny them a patent and was unconstitutional since it was not compliant with TRIPS. It was a strange challenge and it failed because it had no merit. The second challenge that Novarties issued was a more straightforward challenge on the merits of the patent denial. That went up to the Supreme Court that ruled in 2013 decisively in favor of the Indian patent law and the Indian patent system, and clarified to Novartis that their objection held no ground.
My colleagues (Dr. Feroz Ali, Dr. Sudarsan Rajagopal, Dr. Venkata S. Raman & Roshan John) and I published a report studying the impact of the law systematically. We looked at about a decade’s worth of data. We looked at every single pharmaceutical patent that was rejected or granted in India, for patents covering small molecules. We focused on one category of pharmaceuticals called small molecules, which are the overwhelming majority of applications. In general, they cover anything that we think of as a drug (the other category is biologics which cover the more complex molecules; e.g. vaccines are biologics, new medications for cancer are biologics.) What we found is that (1) the patent rejections were robust, patent applications were being rejected at a low rate but with rigor. (2) however when we looked at the patents which were granted, we were somewhat shocked. What we were shocked about is that the law was being disregarded; in fact, we found that 7 out of 10 patents that were granted were in error and in contravention of the Indian patent law.
There are a couple of reasons we think can explain this. The first was the context; there was confusion in how to interpret the law, because of the Novartis case. There is also a degree of confusion because of the wording of the law. In 2005, India had to be careful not to overstep. In many ways, the wording of the law was to hedge bets, to present Indian patent law as less clear cut and radical than it was. What we found was: that attempt to hedge bets and to stay on the right side of TRIPS resulted in massive misinterpretations as well as massive opportunities for applicants to obfuscate the facts. So when you say we need to have this substantive increase in therapeutic efficacy, over 60% as a threshold, that wasn’t really implemented and so when the patent office would say this is just a minor modification, where is the evidence of therapeutic efficacy, the law firms representing the pharmaceutical companies would write back with something, which was not evidence of efficacy but sort of a word salad containing the word efficacy and some evidence of something, which on closer examination should not have passed the threshold but did by accident or omission or error. To us, it suggested that it is time to upgrade Indian patent law, look at the evidence which shows that it has not worked for the most part, and to update it to clarify the original intention of 2005.
Q: In terms of the impact on the ground, in terms of how all of this affects people’s lives, can you describe the case of cystic fibrosis, a debilitating disease that affects young children?
AP: In the United Kingdom, there was a campaign a few years ago, in the runup to the 2019 elections, on access to a medicine called Orkambi which dramatically alters the landscape of life for children with cystic fibrosis, makes their lives better and extends their lives significantly. The NHS, one of the best functioning socialized healthcare systems, was unable to afford this drug. Its manufacturer, monopoly owner, Vertex, was not willing to budge on the very high price that they had set around this drug, and it was outside the boundaries of what the NHS could afford. There was a campaign in the UK to take out “government use” licenses to negate the patent monopoly, so that they could import the drug from other places or manufacture a generic version that would be cheaper.
You would think that the UK would be able to import cheap generics from India. There are many countries that in part or whole rely on cheaper generic drugs from India. Orkambi consists of two compounds – Lumacaftor and Ivacaftor. They are simple to replicate and any manufacturer could make those drugs. But India granted patents on those drugs (under the 2005 law). After those patents were granted, Vertex, the company that applied for those patents, sold 9 quantities in India (yes, you read that right; the quantity of the drugs sold after the patent was granted was 9.) But because those drugs are patented, India cannot also export generic versions of those compounds to the UK. That has meant that India could not be a solution to this problem in the UK even if the UK had taken up these compulsory licenses where they negated the patents on Orkambi. (Vertex finally caved to public pressure and offered the drug at a lower cost.)
Covid Vaccines
Q: Finally, we are having this discussion at the time of the covid19 pandemic, where the issues we discussed are tremendously significant. Can you briefly describe the effects of IP laws that we are already beginning to see on the pandemic?
AP: The international patent system has been left relatively untouched by the pandemic. At the beginning of the pandemic, I expected all vaccine manufacturers, even treatment manufacturers, companies making things like remdesivir, that Gilead holds a monopoly on, regenerative antibodies produced by companies like Regeneron; I expected all these companies to make immediate allowances for multiple production sites, for many manufacturers to come together to make the massive quantities of these things. I expected that because of the early tone that was set by governments in the West and by the pharmaceutical companies themselves. Given the unprecedented nature of the crisis, the unbelievable economic toll, not to mention the incredible human toll in many rich countries, I expected a very different set of allowances for the pandemic. I thought the job of activists at that time, and many others did too, was to extend those allowances to the other things we die off from like cancer, HIV/AIDS, cystic fibrosis, the range of problems where we need the same allowances.
That changed quite early on in the pandemic when it was clear that the system itself was not going to be touched. The allowances would be very few, if any. And in fact, there were no allowances that were made. Of the nine leading vaccine manufacturers in the West, only two have any kinds of access provisions, and those are AstraZeneca, and Novavax, which hasn’t been approved because it hasn’t come to market as yet. The other vaccine manufacturers did not even try to create multiple sites of vaccine production or to license the technology of the vaccines. The vast IP system that protects those monopolies is entirely in place without any change. That’s why I was so interested in supporting the proposal made by India and S. Africa at the WTO to suspend a large portion of the monopolies that are mandated under TRIPS during the course of the pandemic. That proposal is still under way at the WTO. There are meetings happening all through 2021, and it’s possible that a resolution can be found. But the WTO works on consensus. So, every member country of the WTO has to agree on any proposal that they put out. Which means it’s highly unlikely that there will be consensus on this issue, because rich countries and Brazil in this case are adamant about protesting the necessity of this waiver. And that is not a good sign. The developing countries can force a vote and the overwhelming majority of the 164 member countries are in support of it. Over a 100 countries have signaled their explicit support and the rest of them will be in support. But the handful of 5-10 countries that have held out can hold the WTO to hostage. So its future is unclear but it is a very useful dialogue and I am really glad that it’s happening. I think it’s a step in the right direction.
Vaccines are a class of drugs called biologics. And biologics have a whole different apparatus surrounding them. So the IP monopolies like patents are important, when it comes to biologics, but they are not the only important aspect of IP or the only kind of monopoly that vaccine manufacturers hold. So with antiretroviral drugs for HIV/AIDS for instance, you could actually legislate your way to a solution. Countries like India and S Africa had the power in their laws to negate patent protection. And then generic manufacturers on that basis could fairly easily make those small molecules and supply them at a cheaper cost.
The problem with vaccines is that even if we negated IP in the form of patents, we still have IP in the form of what are called trade secrets. The trade secrets are the knowhow, the technology for the production of the vaccine, and sometimes, the cell lines, the very biological material that vaccine manufacturers use to create their approved vaccine. The problem with that is that the regulatory agencies around the world, the Indian drug regulatory agencies, for instance, which are very separate from the patent system, will not really approve a generic vaccine. We do not have generic vaccines in the same way as we have generic drugs. You only have licensed vaccines. So the AstraZeneca licensed vaccine being produced by the Serum institute for instance (just approved by the Indian regulator) is not a generic vaccine. It’s a licensed vaccine which is a different thing. It’s a licensed vaccine because AstraZeneca gave Serum the original cell lines, the entire technology transfer process, and its knowhow, in addition to licensing its patent monopolies.
For Serum to produce a generic vaccine, even a generic vaccine that is exactly equivalent to what the AstraZeneca vaccine is, they would have to go through the entire set of clinical trials, all the way until Phase 3 to satisfy the Indian regulators – which would effectively render it a new original vaccine with a long pathway to approval, not a generic vaccine. It’s the same process in every other country. The only way vaccines can go through an abbreviated process is when they are licenses, like in the case of AstraZeneca. Vaccine manufacturers hold two layers of monopoly protection, and for the second layer of protection which are trade secrets, they will actually have to license those trade secrets, or be compelled in some way, if it’s possible – say, in the United States, by the Defence Production Act – in order for a replica vaccine to be created. And that means that the problems are really steep.
At the moment, we’re putting the lid on a new report that examines how Indian patent law deals with monopolies on biologics, including vaccines, and we look outside patent law, to drug regulation, to untangle the second layer of monopolies that vaccines enjoy. It’s a dense, complex topic, with no easy way out: our legislation, even in India, is ill prepared to even understand the first thing about biologics, and is essentially, shooting in the dark. We hope that the extensive raw data and empirical evidence we present, along with the incredible urgency this pandemic has brought us, might prompt the Indian government to take some radical steps in ensuring this country can produce the vaccines and biologics all of us need to live, within India, and in all the countries across the world who depend on us.
Raghav Kaushik is an activist based in Seattle. His recent engagements have been with the Tax Amazon campaign in Seattle, and the fight against the authoritarian Modi regime in India, specifically the recently passed Citizenship Amendment Act and National Registry of Citizens
GET COUNTERCURRENTS DAILY NEWSLETTER STRAIGHT TO YOUR INBOX