Inaugurating the first Global Innovation Summit of the pharmaceuticals sector in November, 2021, Prime Minister Modi, in his characteristic triumphant style, said, “the global trust earned by the Indian healthcare sector (in recent times) has led to the nation being called the “pharmacy of the world” (https://www.business-standard.com/article/current-affairs/india-is-now-being-called- pharmacy-of-the-world-says-pm-modi-121111801288_1.html).
It is true that the Indian pharmaceutical sector meets 50% of the global demand for various vaccines, 40% of generic demand in the US and 25% of all medicine in the UK. The domestic pharmaceutical industry includes a network of 3,000 drug companies and around 10,500 manufacturing units. India therefore occupies an important position in the global pharmaceuticals sector (https://www.ibef.org/industry/pharmaceutical-india) The country has a large supporting pool of scientists and engineers, who should primarily take credit for this.
Recent setbacks:
Two isolated reports in the recent times about the country’s pharma sector have raised concerns about the intrinsic problems that the sector faces, which, unless addressed urgently and decisively, can pose a serious threat to its dominant role in the global pharma sector.
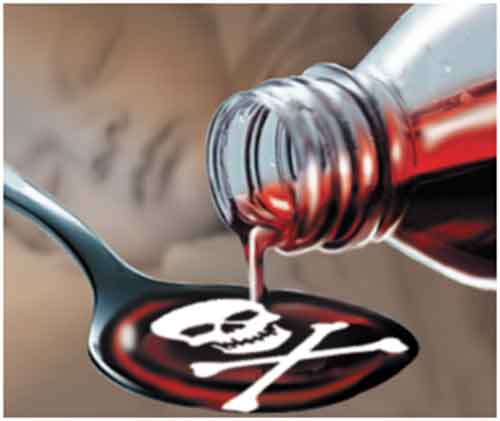
(i) Gambia- Death of 66 children:
66 children in Gambia, who were apparently administered an India-made cough syrup, lost their lives in October, 2022. That brand of cough syrup was supplied by a Haryana-based Indian company, Maiden Pharmaceuticals. The incident caused a nation-wide uproar in Gambia. Heart- rending pictures of grieving mothers appeared in many news papers across the world.
Based on an independent lab analysis of the cough syrup samples, the WHO promptly issued an alert, advising the regulators to stop selling the syrup. The Indian regulators also quickly jumped into action and ordered Maiden Pharma to close down its unit. Questions were raised about the role of the Indian regulators in allowing the export of such a substandard cough syrup. Government labs in India later said that their tests on the syrup found that they were “complying with specifications“.
The Indian regulators said that the WHO was “presumptuous” in blaming the Indian cough syrup. WHO in turn firmly stood its ground.
Meanwhile, a Parliamentary committee in Gambia, after a prolonged investigation, said it “is convinced that Maiden Pharmaceuticals [is] culpable and should be held accountable for exporting the contaminated medicines………………………………………… The findings remain the same with the previous reports which
indicates that Promethazine Oral Solution, Kofexmalin Baby Cough Syrup, Makoff Baby Cough Syrup and Magrip N Cold Syrup were contaminated with diethylene glycol and ethylene glycol.” The committee recommended to the Gambian government that they should not only blacklist the Indian company but also initiate legal proceedings (https://www.bbc.com/news/world-asia-india- 64047948). The committee is reported to have made several attempts during the course of its investigation to contact Maiden Pharmaceuticals but the latter did not respond (https://thewire.in/health/indian-firm-culpable-for-kidney-injuries-linked-to-death-of-70-children- gambia-parliament-probe-says)
The Parliamentary committee’s findings cannot be ignored by the Indian authorities.
While there could be arguments and counter arguments on the culpability of the Indian company, the fact remains that this incident has caused a great deal of damage to the reputation of Indian pharma products.
It is not as though the Gambian case was merely an isolated aberration, that should not lead one to cast aspersions against all Indian medicines.
Maiden Pharmaceuticals itself appears to be a habitual offender, non-compliant with the WHO’s “good manufacturing practices” (GMP), though the company had claimed to be in such compliance. There were at least two States, Kerala and Gujarat, that repeatedly complained in 2015, 2021 and 2022 against the company for supplying substandard medicines but the Central regulator failed to act (https://thewire.in/health/maiden-pharma-gambia-cough-syrup-repeat-offender- substandard-drugs)
In the past several years, there were complaints about cough syrups, diabetes drugs etc. in several States including Delhi, J&K, Himachal Pradesh, Gujarat, Kerala and Tamil Nadu. There were child deaths reported in some of these States. In J&K, twelve children, administered with cough syrup manufactured in Himachal Pradesh, lost their lives during 2019-20, The cases filed against such errant drug companies are still pending.
(ii) Nepal’s ban on Indian medicines:
The second incident is that Nepal banned medicine imports from 16 Indian pharma companies for failing to comply with the World Health Organization’s (WHO) good manufacturing practices (https://www.indiatoday.in/india/story/nepal-bans-medicines-import-from-16-indian-firms- 2311444-2022-12-20). One of the companies so banned figures among those selected by the Indian authorities recently to be subsidised under the Production Linked Incentive (PLI) scheme introduced by the present government to give a boost to domestic production of medicines. While one may question Nepal drug regulator’s action, it is a fact that many pharma units continue to be non-compliant with the good manufacturing practices recommended by the global regulators, including the WHO and the drug regulatory authority of the USA. A senior official of the office of the Drug Controller of India seemed to have admitted this, when he was reported to have said that the Indian market might not be ready to follow global standards and the Indian industry might even collapse with the stringent norms followed elsewhere (https://www.business- standard.com/article/economy-policy/if-i-follow-us-standards-i-will-have-to-shut-almost-all-drug- facilities-g-n-singh-114013000034_1.html).
Global “good manufacturing practices (GMP)”
The question of Indian pharmaceutical industry conforming to GMP cannot be viewed from the restricted point of view of what the pharma industry can do and what it cannot. If there are safety norms globally adopted, which have an impact on the health of the people, they need to be enforced strictly in India, as it concerns the safety of patients.
Drug regulation in India:
The Parliamentary Standing Committee on Health, in their 59th Report submitted to the Parliament in May 2012, examined the role of the Central and State drug regulators and observed, “most of the ills besetting the system of drugs regulation in India are mainly due to the skewed priorities and perceptions of CDSCO. For decades together it has been according primacy to the propagation and facilitation of the drugs industry, due to which, unfortunately, the interest of the biggest
stakeholder i.e. the consumer has never been ensured. Taking strong exception to this continued neglect of the poor and hapless patient, the Committee recommends that the Mission Statement of CDSCO be formulated forthwith to convey in very unambiguous terms that the organisation is solely meant for public health”
The Mission Statement of CDSCO has since undergone a change, as recommended by the Parliamentary Committee, but its role has not changed substantively.
Two public-spirited professionals, Dinesh Thakur and Prashant Reddy, have recently come out with their thought-provoking book, “The Truth Pill”, based on a comprehensive study of the shortcomings of drug regulation in India and its adverse impact on the health of the people (https://blog.petrieflom.law.harvard.edu/2022/11/18/book-review-the-truth-pill-drug-regulation- india/). The authorities in the Ministries of Health and Pharmaceuticals should respond to what they have brought to light.
While the Parliamentary Standing Committee did point out that the drug regulator is more concerned about promoting the pharma industry, than ensuring the safety of the patients, It is perhaps unfair to place the blame entirely on the CDSCO, as those occupying the highest offices in the government are themselves complicit. It is they who fail to enact laws when necessary and tweak the existing laws to suit the industry. It is they who deliberately weaken the regulatory institutions to help the industry. It is they who also display forgiveness towards the pharma units that violate the law of the land. After all, the drug regulator is merely a cog in the wheel of governance!
The Drug and Cosmetics (Amendment) Bill in 2013:
Based on a report submitted by a committee headed by Dr R A Mashelkar, the then head of the CSIR in 2003, the UPA government introduced the Drug and Cosmetics (Amendment) Bill in 2013, for amending the main Act of 1940, for creating a Central Drugs Authority as an independent body to ensure stricter regulation of the pharmaceutical industry. The successor government that came to power in 2014 dragged its feet till June 22, 2016, when the Union Cabinet headed by Prime Minister Modi discussed its implications and decided to withdraw it (https://pib.gov.in/newsite/PrintRelease.aspx?relid=146413). The Cabinet decision was based on the following grounds:
“In order to leverage the comparative cost advantage, the demographic dividend and the advantage in information technology, the Indian medical products sector is poised for exponential growth in the near future and it would, besides meeting the domestic demand, has the potential to become an international hub for manufacturing these products and attracting investment in the sector.
Keeping in view the objective of make in India, it has been decided to comprehensively review the existing law with two fold objectives viz. to facilitate the ease of doing business and substantially enhancing the quality and efficacy of our products”
One would have expected at that time that a well meaning government would further tighten the law by replacing the 2013 Bill by a stricter law to regulate the pharma industry and safeguard the health of the people. It took six years for the government to come up with the new Drug and Cosmetics (Amendment) Bill of 2022, which is more or less a replica of its predecessor legislation, with the exception of bringing medical devices into its ambit, without any mention of an independent central drug regulatory authority committed to safeguarding the health of the people. It fails to address the concerns flagged by the Parliamentary Standing Committee in 2012.
Had the government brought into existence in time an independent, professionally well-equipped central drug regulatory authority on lines similar to the drug regulator in the USA, twelve children consuming substandard cough syrups would not have lost their lives in Udhampur district of Jammu & Kashmir in 2019 and 2020 (https://www.moneycontrol.com/news/trends/health-trends/deaths-in- jammu-due-to-cough-syrup-a-grim-reminder-of-drug-regulation-laxity-4967951.html) and the Gambian tragedy that has raised questions about the safety of Indian drugs would not have taken place.
The plight of the patients:
The Parliamentary Committee (2012) did not mince words, while describing the plight of patients in India in the matter of choosing medicines. In their words,“They (medicines) are the only commodity for which the consumers have neither a role to play nor are they able to make any informed choice except to buy and consume whatever is prescribed or dispensed to them because of the following reasons: Drug regulators decide which medicines can be marketed; Pharmaceutical companies either produce or import drugs that they can profitably sell; Doctors decide which drugs and brands to prescribe; Consumers are totally dependent on and at the mercy of external entities to protect their interests” The patient in India has nowhere to go, as the elected government chooses to be friendly with the industry, condoning its misdeeds, rather than trying to understand the patients’ woes and resolving them.
The nexus between some medical practitioners and some pharma companies is best illustrated by recent income tax searches conducted against a Bangalore-based pharmaceutical manufacturer of a drug used to combat Covid infection, which revealed the group’s use of unethical practices to promote its brands. The charge against the company was that it had in its books, expenses for the distribution of freebies to medical professionals under the heads “promotion and propaganda”, “seminars and symposiums”, and medical advisories. The freebies were worth Rs.1,000 crore and included travel expenses, perquisites, and gifts to doctors and medical professionals. Pharma marketing is governed by the Uniform Code for Pharmaceutical Marketing Practices (UCPMP), which is voluntary and has been in force since 2015. Several civil society organisations had demanded that the Code be made statutory to prevent pharma companies from adopting unethical, people-unfriendly practices, to further their own business interests. Following the Bangalore income tax searches and a CBDT press statement on it, the Federation of Medical and Sales Representatives’ Associations of India (FMRAI) and Jan Swasthya Abhiyaan (JSA), an NGO, filed a PIL before the apex court for making the Code statutory and binding. While the conduct of doctors is covered by the Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002, under the Indian Medical Council Act, 1956 and the National Medical Commission can cancel the errant doctors’ licenses, the pharma companies cannot be proceeded against (https://frontline.thehindu.com/the-nation/public-health/dolo-controversy-revives-demand- for-regulating-pharma-marketing-practices/article65949470.ece) Instead of recognising the merit of the arguments put forward by FMRAI and JSA in the PIL cited and informing the court that it would make UCPMP statutory, the Ministry of Health filed a counter, defending the present non- enforceable UCPMP ( https://frontline.thehindu.com/the-nation/public-health/dolo-controversy- revives-demand-for), apparently caving in to Indian Pharmaceutical Alliance (IPA)’s demand, as expected, relegating the public interest to the background.
The pharma industry’s ugly pollution footprint:
In terms of the pollution havoc they wreak, the pharma manufacturing units remind one of the good old Charlie Chaplin’s memorable action in the 1921 film, The Kid. The Kid throws stones to break windows so that the Tramp (played by Charlie Chaplin), working as a glazier, can be paid to repair them, both making easy money (https://www.youtube.com/watch?v=Ue1tQ8NJHTs). Likewise, the pharma units are polluters on one side, damaging the health of the people, who live in their vicinity and they produce expensive medicines required to treat the people for their health problems.
It is ironic that the Centre and the States should spend thousands of crores of rupees for providing healthcare for the people and, at the same time, facilitate industrial units including the pharma industry to pollute and cause health problems. The reason for this is that there is a strong bond of bon homie between most political parties in India and promoters of many pharma units. The latter, like their counterparts in other sectors, provide electoral donations to political parties, in exchange for the former tweaking the laws in their favour, once they come to power ((https://www.business- standard.com/article/economy-policy/data-shows-bjp-bagged-92-of-corporate-donations-to- political-parties-119011701405_1.html). As a result, once in power, the political parties lose no
time in twisting the laws and regulations to suit the industry, weakening regulation and displaying forgiveness towards the polluters, who violate the law.
According to an analysis (https://thewire.in/environment/throughout-the-pandemic-environmental- clearance-law-has-been-under-the-chopping-block), during the last few years, 33 changes were made in environmental regulations; seven were made on the pretext of the pandemic. They included extension of the terms of the central and state expert appraisal panels and authorities, extension of validity of existing environmental permissions of projects and exemptions to the pharmaceutical sector. Every such permission or concession entails a corresponding long-term damage to the health of the people, for no fault of theirs. It is ironic that the Environment Ministry should resort such manoeuvring in stealth, under the pandemic cover.
The Ministry of Environment has a long list of accredited consultants who are qualified to carry out environment impact appraisal (EIA) studies for industrial units, on the basis of which the Ministry accords statutory environment clearance. A cursory look at the list reveals that some of those consulting companies are owned by promoters of pharma units, which clearly involves a conflict of interest. No wonder, that one often comes across such EIA consultants churning out studies in favour of the industrial units that they are expected to appraise objectively, often copying and pasting portions from one study to another, in a casual and a blatant manner, as they know for certain that the Ministry would wink at it. The Ministry considers such calculated forgiveness “promoting ease of business”!
Wastes from pharma units pollute water bodies in the country on a large scale.. A recent global study (https://www.pnas.org/doi/pdf/10.1073/pnas.2113947119), based on an analysis of the sewage let out in cities across the world, found that a cocktail of 22 active pharma ingredients (APIs), including metformin, in river water samples collected in the capital region of Delhi (https://india.mongabay.com/2022/10/humans-are-contaminating-earths-waterways-with- medicines-pharmaceutical-ingredients/#:~:text=A%20study%20published%20in
%20June,40%25%20of%20sites%20tested%20globally). Based on a comparison of the cumulative API concentrations detected across 137 river catchments, the global study places India among the top four countries in the order of descending pollution levels. This should give us an idea of the magnitude of pharma industry’s pollution reach.
There are large pharma clusters located in States like Telangana and Andhra Pradesh, where it a common sight to come across water bodies contaminated with wastes and unbearable stink permeating the surroundings. The common effluent treatment plants set up with government subsidies rarely function to their full capacity and promoters of some pharma units choose to cut corners, to maintain their profits, by dumping the wastes on vacant lands and in water bodies.
Groundwater aquifers near many pharma units get contaminated with chemicals from pharma wastes.
Industrial safety record:
The pharmaceutical industry has been notified as one involving hazardous processes (https://dgfasli.gov.in/en/book-page/list-industries-involving-hazardous-processes). In an environment of all-round forgiveness and business friendliness across the country, rarely do the concerned authorities make sure that pharma units observe the prescribed safety norms and ensure the safety of their workers and the safety of the people living in their vicinity.
To cite an example, in a pharma complex known as Jawaharlal Nehru Pharma City (JNPC) near Visakhapatnam in AP (https://visakhapharmacity.com/) housing more than 90 individual pharma manufacturing units, apart from the pollution stink it generates all around with its associated problems, the occurrence of accidents is more a rule than an exception, and many accidents are fatal. One randomly accessed local news report that appeared on July 15, 2020 (https://www.newindianexpress.com/states/andhra-pradesh/2020/jul/15/visakhapatnam-fire-mishap- five-accidents-within-seven-months-in-pharma-city-2169944.html) read as follows:
“In the last seven months, five accidents occurred in the Pharma City, in which seven persons were killed. On June 29, two persons died and four others were injured due to hydrogen sulphide leak at Sainor Life Sciences. In the same plant, a major accident occurred in 2015.
In a mishap at Smilax pharma, two persons died on December 27, 2019. Just a day before, one person died and 10 fell ill due to gas leak at Smilax unit. In 2019, one person died at Alkali pharma when he fell down while doing centring work on the first floor. At Actis generics plant, one person died after a fall while doing painting work”
The people of the northern part of AP are accustomed to see such reports every now and then. They know that the authorities responsible for ensuring industrial safety wake up after each accident for a make-believe post-mortem quick response, forget it in a few days, to wake up once again, when the next fatal accident takes place. The families of the workers who have lost their lives in those accidents are easily forgotten. Meanwhile, not a single promoter of an accident-prone pharma unit is arrested and brought to book. This is perhaps the sad story about most such pharma complexes in the country.
Should not the pharma industry set its own house in order?
Following the tragic incident such as the one that took place in Gambia, and the rebuff given by Nepal, neither the government at the Centre nor the pharma industry in India, can continue to adopt an ostrich-like approach, closing their eyes to an under-regulated environment in which the industry is allowed to cut corners on many fronts, that forces them to leave an ugly domestic footprint of substandard medicines, environmental damage and unsafe workplaces. While the industry, under those circumstances, may take short leaps of progress, it will certainly stumble in the long run, unless corrective steps are taken now.
E A S Sarma, Former Secretary to Government of India