Co-Written by K. Rajasekharan Nayar and Arathi P. Rao
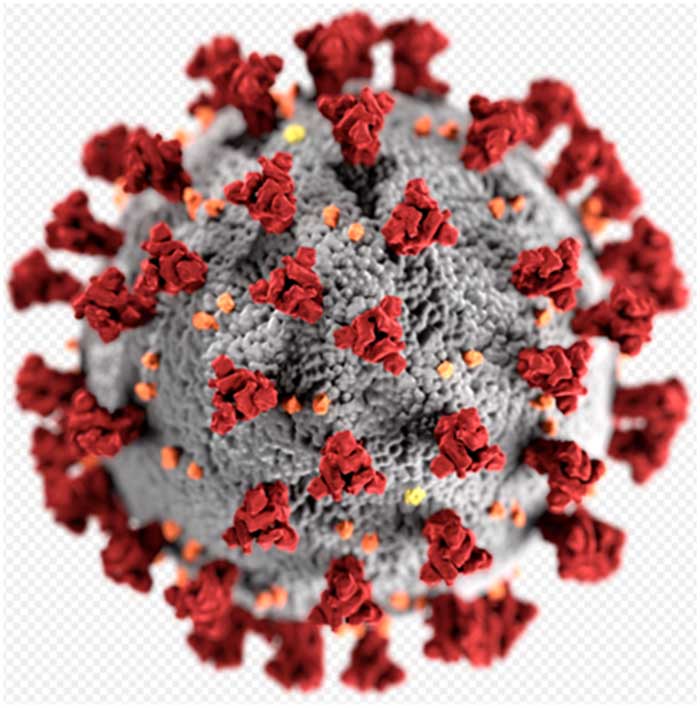
The possibility of developing vaccines and drugs against COVID-19 is being closely watched by the world. The journal ‘Nature’ reports that there are about 115 vaccine development initiatives in the world of which 78 are confirmed as active and 37 are unconfirmed and of the 78 confirmed active projects, 73 are currently at exploratory or preclinical stages. It is still only a distant possibility that a vaccine will be made available in the near future. ‘Nature’ states that strong international coordination and cooperation between vaccine developers, regulators, policymakers, funders, public health bodies and governments are needed to achieve the target.
The availability of drugs perhaps is less uncertain with pharmaceutical companies and their research stations wanting to exploit the situation at a short notice. The probability of drug development is high as there is more market and therefore more profits in this field. There were also efforts to test the possible effect of chloroquine/hydroxychloroquine against SARS-CoV-2 since this was previously described as a probable inhibitor of most coronaviruses, including SARS-CoV-1. Initial trials of chloroquine in the treatment of COVID-19 have been encouraging but the possible mechanisms of chloroquine interference with the virus replication cycle is yet to be revealed. And some trials on the effectiveness of the drug had to be stopped after initial problems especially because patients experienced side-effects.
The experience of Dengue and Chikungunya is important in this context although they are Vector Borne viral Diseases(VBD) unlike COVID-19 which is a droplet infection. They are also important because of the arrival of monsoon season which is also the time for viral infections. Dengue, with its 4 serotypes of virus has thrown several challenges in the past for development of a vaccine. The viral infection has demonstrated varied influences on the immune system of the infected host. Primary infection stimulates antibodies which initially neutralise the infection, but with time, they become cross reactive facilitating the entry of the viruses of other serotypes into the host cells. This type of cross reactivity has been found in humoral as well as cell mediated immunity in these infections with manipulation of the host antiviral response. There has been evidence to demonstrate the involvement of immunity in severity of manifestations like haemorrhagic fever and shock syndrome. Autoimmunity has also been suspected in a few cases. Different subsets of population can have different experience of the VBD epidemics. Primary infections have been found in infants of mothers who had dengue previously. Adolescents have acquired dengue infection of a different serotype due to the seroprevalence.
The major limitation with respect to viral infections especially that of COVID-19 in developing a vaccine is that there are huge unknown components and probably different strains. The classic example in the history of disease in the modern world is with respect to the Influenza pandemic of 1918. It was not until the 1930s that researchers established that influenza was in fact caused by a virus, not a bacterium. And many vaccine development initiatives since 1918 failed because of this unknown fact. Even with respect to pneumococcal bacterial infections, the vaccine developers were not able to identify all the potential disease-causing strains of the bacteria. The pneumococcal vaccine for children available at present protects against 13 serotypes of that bacteria, and the vaccine for adults protects against 23 serotypes.
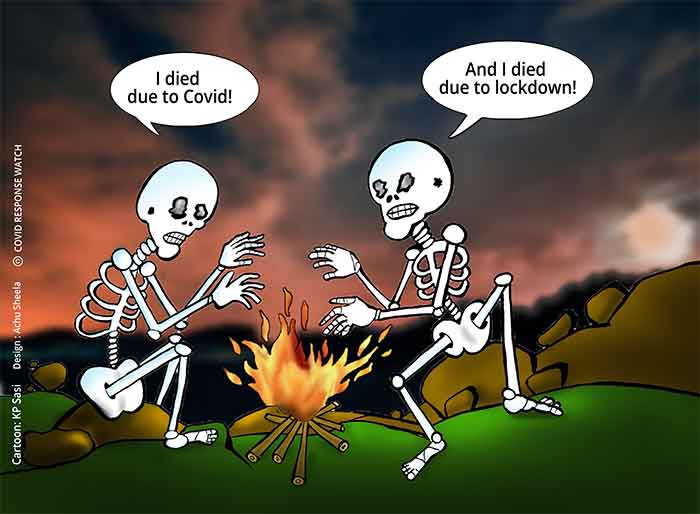
There are also reports regarding the presence of different strains of COVID-19 virus. One would want to believe that it is the same strain which reached these shores and infected humans. The issue of herd immunity to the virus is another issue which is vital and which the world is looking forward to. The earlier virus infections like the Influenza pandemic of 1918 lasted for almost two years although most of the mortality was packed into three months. It gradually disappeared and we do not know the real reasons for the same. Herd immunity is less likely compared to evolution of less lethal strains of the virus but these are just assumptions. Another possible reason is the effective, non-pharmaceutical interventions (NPI) like the ones being practiced in the present pandemic. With respect to COVID as well, these assumptions, especially evolution of new mutated strains are the biggest stumbling block for developing vaccines. An effective vaccine or even drugs against the virus should not be the focus at the moment.
The current focus needs to be on immunity as the monsoon has reached the shores. Immunity boosters or maintenance by preventing co-infections is the only temporary weapon against COVID-19 for which the herd lacks immunity. If the endemic VBDs which has every possibility to resurface in the present season and impacting the host immunity, it could make the population more vulnerable to the pandemic. It is observed that there are some problems in distinguishing between Dengue fever and COVID-19 because they share clinical and laboratory features. It has been found in several countries that cases which were wrongly diagnosed as dengue were later confirmed to be COVID-19. Accuracy of diagnostic tests is certainly an issue and failure to test diseases could have serious implications for the state of public health. Countries and states in India with fragile health care infrastructure and poor service delivery mechanisms would not be able to handle a co-existent epidemic with a pandemic crisis. Many of the resource limited settings across the globe works on redistribution of health care resources on a demand-supply basis, hence, would fall short of expectations in a co-existent disease scenario which needs to be handled carefully
(Professor Kesavan Rajasekharan Nayar is affiliated to Global Institute of Public Health, Ananthapuri Hospital and Santhigiri Research Foundation, Thiruvananthapuram. [email protected]; Dr. Arathi P. Rao is affiliated to Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal. [email protected])
Resources:
https://www.historyofvaccines.org/content/blog/spanish-influenza-pandemic-and-vaccines
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7144614/
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30158-4/fulltext
SIGN UP FOR COUNTERCURRENTS DAILY NEWS LETTER